You may have seen multiple articles out there that describe myocarditis after COVID vaccination and how you should be concerned about it. There are many layers to the diagnosis of myocarditis, and I as a board-certified pediatric cardiologist, wish to share with you some of those layers of nuance.
This article will focus on myocarditis as a disease from the perspective of the mainstream pediatric cardiologist – for excellent articles on the research methodology related to postvaccine myocarditis and statistics, I refer you to the excellent previously-written work on Science Based Medicine by Dr. David Gorski, Dr. Dan Freedman, and Dr. Jonathan Howard.
The heart, myocarditis, and complex etiology
Many news sources at this point have tried to make the case that COVID vaccine myocarditis is worse than COVID disease myocarditis. To understand where this assertion comes from, one needs to begin with some definitions. The heart muscle is composed of many different types of tissue, including connective tissue (scaffolding), muscle tissue (the workhorse), nerve tissue (the communications network), electrical tissue (for communication inside the heart), and vascular tissue (to keep everything fed). Myocarditis at its core is inflammation of the heart. There are many, many causes of myocarditis, and because myocarditis appears to happen after vaccination in mostly kids and young adults, I will focus my discussion on this group. The risk-benefit ratio in older adults is much, much more clear.
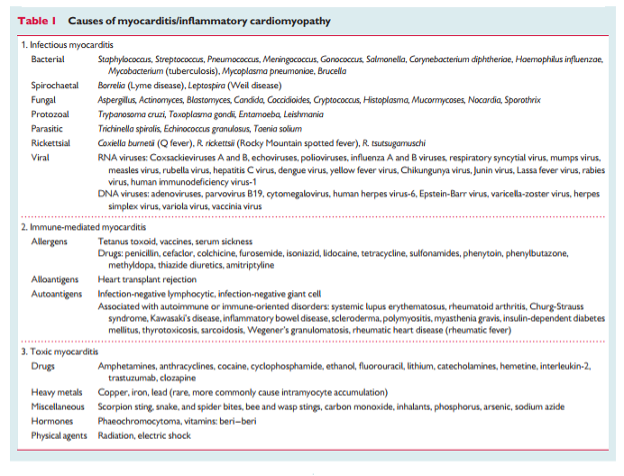
Kids can get myocarditis from many different sources, but most kids generally get myocarditis because they were exposed to a virus of some variety. Here are only a few of those causes (citation: European Society of Cardiology):
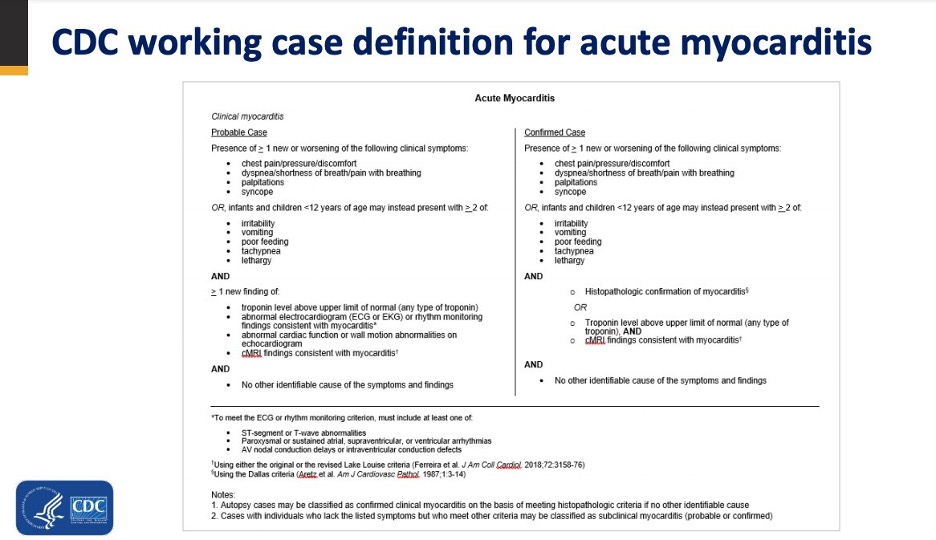
Myocarditis is typically diagnosed in the Cardiology office or hospital setting with the following case definition by the Centers for Disease Control and Prevention (with small regional variations):
Just looking at the cases of reported myocarditis can be quite disheartening to the non-medical reader. The next question is naturally, why didn’t the mRNA platform vaccination get paused immediately after all these cases of myocarditis were found? Weren’t the adenoviral vector platform vaccines paused right after the discovery of vaccine-induced thrombotic thrombocytopenia? Well, if you don’t remember anything else – I would emphasize that not all myocarditis is of the same severity. Why didn’t myocarditis feature prominently in the core clinical trials? It wasn’t because the researchers weren’t looking, it’s because of a concept known as study power. If a fluorescent needle can only be found in 1 in 100 000 haystacks, many haystacks must be searched to locate the needle. If the needle lives in 1/50 haystacks, the search is much easier.
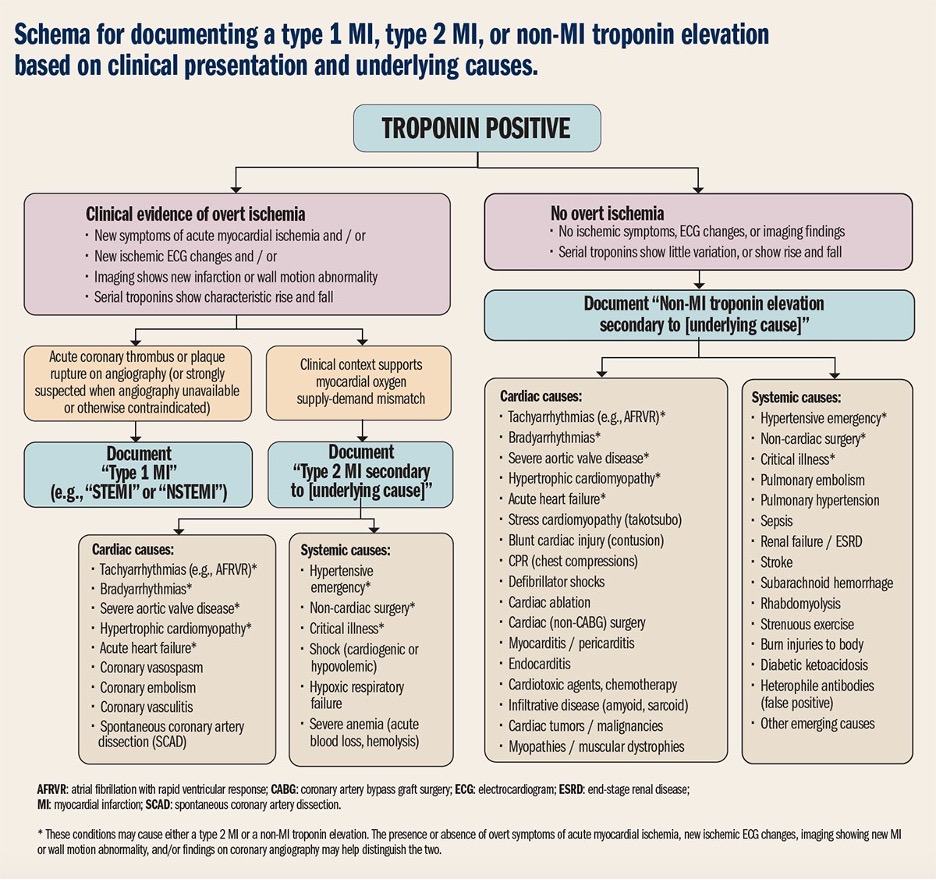
The historical incidence of myocarditis of all causes is estimated at around 1-2/100 000 (citation: Moss and Adams Heart Disease in Infants). Myocarditis historically has been diagnosed slightly more in men than in women. The classic blood test used to look for myocarditis is troponin, which is a normal component of the heart muscle. The problem with just labeling every patient who has troponin in the blood as a “myocarditis” is that not all that bleeds troponin, is myocarditis (citation: American College of Cardiology):
It is a cardiologist’s role to help sort out which patients have genuine myocarditis, and which patients have a higher troponin level in the blood due to some other cause (which could be something as simple as a football match). The diagnosis of myocarditis can also sometimes be difficult! There is a saying in medicine – patients don’t always read the textbook. This means that patients rely on us to figure out why their body has done something unusual, and they don’t always directly fit the traditional list of characteristics that we were taught to search for in medical school. When the diagnosis becomes difficult, cardiologists or radiologists specializing in cardiac MRI can come to the rescue – and image the heart. (Image citations UCDavis and Auntminnie.com). There are specialized MRI criteria that cardiologists use to help confirm the diagnosis.

An MRI machine…
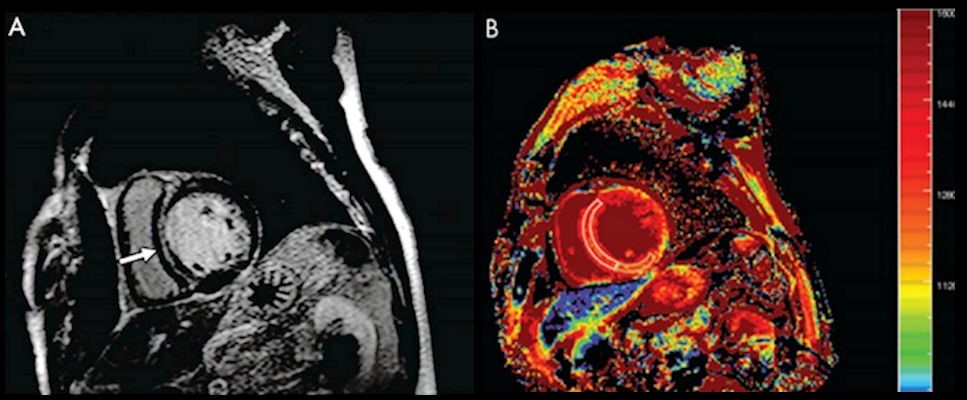
…and the image it produces.
Cardiologists can use the combination of how the patient is behaving, the EKG, echocardiogram, lab tests, and cardiac MRI (if available) to triage the severity of the illness. Not all hospitals may offer cardiac MRI, and sometimes you may observe a cardiologist making use of the other tests that are available in that particular hospital’s toolkit. Every discussion of COVID vaccine myocarditis versus COVID disease myocarditis must include a description of their comparative severity otherwise that discussion can very easily be misleading.
What is known about COVID vaccine versus disease myocarditis?
The real incidence of viral myocarditis from all seasonal viruses in young men is a little difficult to calculate but is probably higher than the numbers quoted above. Why? Because every patient with a sniffle doesn’t see a cardiologist to figure out if there is myocarditis, and rightfully so. It’s reasonable to match your depth of testing with the severity of the disease. The severity of viral myocarditis ranges from being symptom-free, all the way up to requiring life support. The same can be said about SARS-CoV-2 viral myocarditis.
In teenage boys and girls, who are most at risk of post-vaccine myocarditis, what is the rate of COVID-19 viral myocarditis versus COVID-19 vaccine-induced myocarditis? From this pre-print out of Cleveland, using the TriNetX Research network, 876 per million boys developed myocarditis overall, and split into 12-15 versus 16-19, those rates were 601 and 561 per million respectively. For the girls, the rates were 213 per million overall, and 235 per million and 708 per million in the 12-15 versus 16-19 age groups respectively. According to the same study, myocarditis after infection is 6 times more likely than after vaccination. According to this 2nd article, which surveyed side effects after COVID infection versus COVID vaccination (albeit in an older age group), the incidence of all the side effects that mattered were worse in the patients who were infected with the genuine virus than vaccination. It was also acknowledged that the vaccination poses an increased risk above baseline of myocarditis. Again – COVID illness myocarditis is a bigger bad actor than COVID vaccine myocarditis.
The now-infamous study authored by Høeg et al is deeply misleading; their core premise is that vaccination myocarditis occurs at a higher rate than in those who get COVID disease. If you purely look at VAERS reports without doing any other analysis, this is the unusual conclusion you will arrive at. VAERS in fact, specifically instructs the reader to not use their database in this way; it is meant as a tool to generate hypotheses, not to search for causality. Databases such as the Vaccine Safety Datalink are much better databases to research this problem. The Centers for Disease Control and Prevention use very specific myocarditis criteria (which aligns with what most cardiologists use) to be as certain as possible, that cases are being estimated as accurately as possible.
All myocarditis is serious, including vaccine-induced
At no point do I wish to downplay myocarditis – if I were to meet a patient with COVID vaccine myocarditis who was deathly ill, I would announce it to the world, and warn everyone of the risks. I thankfully have yet to meet such a patient, and the patients that are in my clinic have all recovered. In my entire clinic, comprising all my cardiologist partners, I have counted approximately 5 total COVID vaccine myocarditis cases. I have similarly asked many colleagues about their experiences, and the consensus is that they are uniformly symptomatically recovering. Although this study had not collected many MRIs by the publication deadline, the study group is going to do a follow-up work that contains MRI studies. The patients in my clinic who are recovering from post-COVID vaccine myocarditis have cardiac MRIs that look very, very reassuring. Some unpublished data exist of patients who have had very concerning cardiac MRIs after COVID vaccination in the absence of documented COVID infection – each of those patients has cardiologists who are watching these patients very carefully. The CDC has convened a specific study group to monitor these patients. This is not the work of an organization that wishes to downplay myocarditis.
Conclusion: Worry about the virus, not the vaccine
I support all efforts to mitigate the risk of mRNA vaccination myocarditis, but given the accelerating Pediatric Intensive Care Admissions, I would be against any effort that attempts to do this at the cost of vaccination efficacy or at the cost of even more PICU admissions. PICU admissions, even if they don’t result in serious long term complications, represent a significant hit to a teenager’s quality of life. I appreciate the efforts of Professor Shane Crotty’s group in elucidating the relative effectiveness of natural immunity versus immunity post-immunization, and eagerly await the Immunology community’s discussion on this hot topic. I won’t claim to be able to expertly interpret their studies and will refer you to them for their perspective. In the end, the risk of COVID vaccine myocarditis is larger than vaccination with many classical vaccines, but the absolute risk is still very, very small – and far smaller than the disease itself. You are trading in a significant risk for a much smaller, calculated risk and pediatric cardiologists are ready to give the necessary care to each patient who may have this complication.