Last time out I caught readers up to speed regarding my thoughts on chiropractic care, particularly when it involves the pediatric population. As I stated in that post, the most egregious example of chiropractors practicing far outside of what would be considered an appropriate scope of practice by any rational outside observer is newborn chiropractic. I linked to several posts that I have written tackling this subject. This will be another one and it should make you angry.
In the October issue of the Journal of Pediatric, Maternal & Family Health – Chiropractic, a vertebral subluxation-focused repository for all manner of pseudoscience, there is an article with a gorge-elevating title: “Resolution of Abnormal Pulse Oximetry Measured in Real-Time in a Neonate with Vertebral Subluxation: A Case Report”. To give a little perspective on the quality of this journal before I delve into this train wreck of a case report, Barbara Loe Fisher is on the editorial board. So is Christopher Kent, president of the Foundation for Vertebral Subluxation.
The case, such as it is
The report in question is bad. It paints a clear picture of a “certified” midwife (certified how?) and a chiropractor with a poor grasp of newborn physiology fumbling their way through the care of a baby immediately after delivery. In the report, the authors, one of which I assume is also the chiropractor involved in the child’s care, focus on one very serious potential cause of low oxygen levels in a newborn, congenital heart disease, completely ignoring other possible etiologies. What they describe is reckless and they are extremely lucky that the baby ended up doing well despite the chiropractic intervention rather than because of it. This report serves as further evidence that chiropractors should not be allowed to treat children.
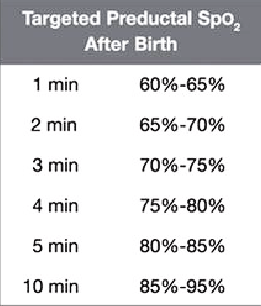
The report begins with the “natural” home birth (another topic for another time) of a full-term 8-pound baby girl after an uncomplicated pregnancy. For an unexplained reason, the midwife placed a pulse oximeter probe on the child’s foot and at 3 minutes she saw that it was reading 73%. According to the authors of the paper, the normal value should be 95-100% and they were seeing continued fluctuations between 80% and 90%. I’ll point out here that it is not the standard of care to start continuous monitoring with oximetry after the uneventful delivery of a term baby, so something may have worried the midwife or it may be something she does with every home delivery. It isn’t entirely clear, but I think I might know the answer.
What is an APGAR score?
The midwife assigned APGAR scores of 7 at both one and four minutes after delivery. APGAR scoring is a fast and simple assessment of a baby’s health during the first several minutes of transition from fetal to newborn physiology, a process that is very complex where a lot can potentially go wrong. It’s a backronym based on the name of Dr. Virginia Apgar, a pioneer in neonatal medicine who developed the scoring system in 1952. It stands for appearance, pulse, grimace, activity, and respiration. Scoring is typically done at 1 and 5 minutes, not 1 and 4 minutes as described in the case report, and then additionally at 5 minute intervals until a baby is stabilized, they require resuscitation, or 20 minutes have passed.
While its utility has its limits because components of the scoring are subjective, there are issues with inter-rater reliability, and it doesn’t predict long-term outcomes, it is a not terrible way to standardize how we decide which babies need intervention and which can go straight to mom. I’m sorry if it sounds like I’m not a fan, but I’m not a fan. I frequently joke with learners that it is the most useless thing we do in medicine. Also whenever I see scores of 10, I know it’s either somebody’s first day in labor and delivery or it’s the baby of a VIP. All babies have blue hands and feet at 1 minute and lose a point for it. And 99.999% of babies have blue hands and feet at 5 minutes. Accept it and move on.
Back to the case…wait, more about APGAR scores
So the baby is found to have low oxygen levels (just play along for now), as determined by pulse oximetry, at 3 minutes. And the APGAR score is 7 at 1 and 4 minutes. They don’t break the scores down, but it’s most likely 2 off for color (central and acrocyanosis) and 1 off for tone (a bit floppy) at 1 minute. I don’t for one second trust the ability of the midwife to determine normal tone in a newborn, however. But in general, an APGAR of 7 at 1 minute is pretty normal. The 5 minute APGAR is where the money is, but it’s bitcoins.
It’s hard to say what they took off for the 4 minute APGAR, which again isn’t when we would typically do the second assessment. The second score is thought of as a snapshot of how well we did our job resuscitating a newborn and it is usually higher or at least the same as at the initial assessment. Typically a baby pinks up centrally and would have better tone, heart rate, and reactivity after some good stimulation or help expanding the lungs a few times with positive pressure ventilation using a bag and mask. But in general, a 7 at 5 minutes is still reassuring.
The authors don’t describe central cyanosis in the report, which would be concerning at this point and unlikely to be left out if it had been present. They also don’t mention anything about the respiratory effort or the heart rate. I have to think that if the baby wasn’t breathing or didn’t have an adequate pulse, they would have commented on it. So maybe they took off a point for color, a point for poor tone, and a point for decreased response to stimulation. If the baby had been blue all over it would at least explain why the midwife broke out the pulse oximeter, but the report implies that it was put on immediately after birth and not in response to concerning exam findings. Honestly, it’s almost as if the people writing this case report don’t know what is important to pay attention to and to document. Weird.
Okay, now back to the case
The midwife then puts the baby on oxygen “intermittently”, but the authors do not explain how this is accomplished. Most likely it was “blow-by“, when an oxygen source is placed near a baby’s face rather than delivering it with a mask, nasal cannula, or endotracheal tube. This method does often seem to do the trick with the little ones, but it doesn’t actually do much to increase the fraction of inspired oxygen above the room air value of 21% unless done in a particular way. Often the blow-by is just somewhere around the baby’s head or chest (or feet), which is useless.
The authors go on to state that after starting the intermittent oxygen therapy, the baby’s pulse oximetry readings increased to 93% to 95% but would sometimes still dip down to 85%. They attributed these dips to when the baby wasn’t getting oxygen, but I’m not confident that the baby was getting any appreciable amount of extra oxygen at any point. They do not provide any additional details on how much time has passed, but they do write that the parents of the child were told that she might need to be transported to a local emergency room because of possible congenital heart disease.
Imagine how scared the family must have been. Now imagine how this family had put their trust in the midwife and expected a competent professional trained to treat the mother and also manage complications with the baby…at home. And then further imagine that someone had the idea to call in a chiropractor. Finally, if you have any remaining neurons not taken over by rage, imagine that the chiropractor, after being told that there is a baby that might have a life threatening heart defect, thought it was within their scope of practice and headed on over.
Enter the chiropractor
I’ll just quote directly from the paper here:
After an in-depth consultation with the parents and the attending midwife, a pediatric chiropractor evaluated the newborn for the presence of vertebral subluxations. Special attention was placed on the upper cervical spine as it is a common area of trauma during the birth process. It is important to understand that even when pediatric cervical injuries in general are a rare occurrence, birth related neck trauma is many times unpublicized and therefore not treated accordingly.
Taking a step back for a minute, let’s look at this rationally. Assuming that they are correct in their use and interpretation of newborn pulse oximetry (be patient, I’ll get there), we have a baby with low oxygen levels requiring oxygen support during the first few minutes after delivery. And the midwife is worried enough about the possibility of congenital heart disease, which in some forms can result in rapid decompensation, shock, and death without immediate intervention, that she is discussing emergency transport.
I’ve personally seen a baby go from well-appearing to critically ill in a matter of minutes as their heart lost the ability to provide oxygenated blood to the body and it is very scary. It’s one of many reasons why home births are a bad idea. How much time was wasted while waiting for the chiropractor to arrive and provide an “in-depth consultation”? The authors go on to describe the chiropractor’s nonsense evaluation of the newborn, which consisted of the standard palpation and leg length checks used by NUCCA practitioners who focus on the upper cervical spine. How long did this take? Again, every second counts if congenital heart disease is a possibility.
To absolutely nobody’s surprise, a vertebral subluxation of the left atlas transverse process was discovered and then “treated” with a “gentle sustained-contact type of force with the middle finger”. The argument being that the amount of pressure one would use to check for the ripeness of a tomato, a very popular description used by baby chiropractors, is enough to move spinal bones around. To their amazement, the chiropractor/author witnessed a real time increase in the baby’s pulse oximeter reading to 95%, and it remained there. Correction was achieved and the baby did not need to be moved to a hospital. Hallelujah!
Let’s break all this down.
Newborn transition and the role of pulse oximetry
I’ll just stick to the cardiorespiratory system of term healthy newborns for this discussion, which is complicated enough without getting into how it is impacted by prematurity. Plus the baby in the report was term. As I mentioned above, a lot of complex physiology is happening just before, and in the immediate period after, a baby is born. This will just be a shallow dive though.
Fetal lungs, which are collapsed and fluid filled, do not receive much blood flow because of high pulmonary vascular pressures, so a fetus receives oxygen from its mother via the placenta. The oxygenated blood coming from the placenta is routed through the inferior vena cava and into the heart’s right atrium where at least half of it shunted away from the right ventricle. The blood instead passes into the left atrium through a hole in the wall between the two chambers (the foramen ovale) because the higher pulmonary pressures make it the path of least resistance.
From the left atrium, the oxygenated blood moves into the left ventricle and then is pumped into systemic circulation via the aorta. In addition to forcing blood across the foramen ovale, the high pulmonary pressures also force about 90% of the blood that did manage to make its way into the right ventricle and pulmonary artery into the aorta through a connection called the ductus arteriosis. So ultimately there is only just enough blood entering into the pulmonary circulation to oxygenate that tissue and the rest goes through the aorta to deliver oxygen to the rest of the body. This is if everything is hooked up correctly.
As labor begins, there is a surge of hormones that signal the lungs to prepare to absorb the fluid within the airways. Within seconds of birth as a baby takes their first breaths, the lungs expand and rapidly clear themselves of the bulk of the residual fluid so that normal ventilation and respiration can occur. This, and the clamping of the umbilical cord, reduces the high pressures within the pulmonary circulation and increases blood pressure in the systemic circulation respectively. As a result, blood flow to the lungs begins to increase because less of it is shunted across the foramen ovale or through the ductus arteriosis, and the lungs replace the placenta as the sole source of oxygen.
The transition that I’ve just described is a gradual process that takes several minutes to occur, thus oxygen levels do not reach “normal” adult values for at least 10 minutes after delivery. And again, this is if everything goes right. Although not needed for normal postnatal circulation in a healthy newborn, these accessory pathways continue to exist for weeks (for the ductus) to months (for the foramen ovale). Sometimes their persistence can cause problems, particularly the ductus arteriosis in premature infants, which may need to be closed with medications or a procedure. Sometimes their persistence is the only thing keeping a baby alive in the case of certain congenital heart defects where the only way a baby is able to get oxygen to the systemic circulation is through these shunts. We sometimes give a medication to keep the ductus from closing until surgery can be performed.
SpO2 is oxygen saturation determined by pulse oximetry.
Pulse oximetry is a very helpful tool in our approach to managing newborns at the time of delivery, and not just for the detection of congenital heart disease. It is based on the absorption of specific wavelengths of light (red 640 nm and infrared 940 nm) by hemoglobin molecules that do or do not have attached oxygen. A probe attached to the skin at strategic locations will measure these values and the device uses the power of math to determine the oxygen saturation. This gives us a much more sensitive means of determining low oxygen levels since we don’t have to rely on the visual assessment of cyanosis, and it is much faster than sending blood to the lab for analysis.
Regarding congenital heart disease, it is now standard to check oxygen saturation percentages in all newborns prior to discharge, typically at around 24 hours of life. There are, however, other potential causes of abnormally low values, such as pneumonia, retained fetal lung fluid, persistent pulmonary hypertension, aspiration of stool passed prior to delivery, and anatomical abnormalities, to name just a few. Many newborns have low values that gradually improve over the first several minutes to few hours that are, with hindsight and often a few reassuring tests, attributed to ultimately benign delays in the normal transition that I described above.
Pulse oximetry is far from perfect, however, and I see false alarms all the time. You can’t just slap it on a baby and expect reliable results. You have to do it right. It can be misleading even when everything is done correctly because the value on the monitor tends to jump around…a lot, leading to frequent false alarms and unnecessary interventions. The probe often loses the signal and many medical professionals don’t realize that oxygen saturation displayed on the monitor is an average over the previous 8 to 16 seconds, so it can take time to represent the actual physiological state of the patient. You really have to know what you are doing when interpreting pulse oximetry in any patient, especially a newborn.
Conclusion: What really happened
As I mentioned earlier, and this is demonstrated in the above table, a healthy newborn’s oxygen saturation starts low and gradually increases during the first ten minutes after delivery. So the oxygen saturation of 73% at 3 minutes described in the case report was very likely completely normal and not representative of an underlying congenital heart defect. And with the reassuring APGAR scores and lack of any mention of red flags such as labored breathing or persistent central cyanosis, this baby was probably perfectly fine.
All the jumping around of oxygen saturation values they described was likely just pulse oximetry doing what pulse oximetry does and they didn’t know how to interpret it. If the baby truly did have abnormal oxygen levels caused by serious pathology such as congenital heart disease, the delay in seeking appropriate care could have resulted in a very bad outcome. It is beyond irresponsible to attempt a trial of chiropractic before calling an ambulance when you are managing a potentially very sick newborn, which is something you would think would go without saying. But here we are.
We use our understanding of human physiology to avoid overzealous use of oxygen when caring for newborns because it can actually be harmful, particularly for premature infants. Before we developed this understanding, this seemingly benign intervention injured the brain, eyes, and lungs of countless newborns. We now know that most newborns can be resuscitated using room air. When we use oxygen, we typically start low and increase the amount to only what is needed to maintain normal oxygen saturation. Only for the small percentage of babies that don’t respond to lower amounts of oxygen, or who require interventions such as chest compression and the placement of an endotracheal tube, do we use 100% oxygen.
In the conclusion of the case report, the authors state that obstetric healthcare providers should know about cases such as this. I agree. I think more people should definitely be made aware of how dangerous the chiropractic profession can be when their delusions of bogus spinal abnormalities put children at risk of very real harm.
One more thing…
Anyone who reads SBM regularly knows how obnoxiously vague and nonsensical the attempts by quacks to science up their belief system can be. My favorite has always been this chiropractic definition of a subluxation:
A complex of functional and/or structural and/or pathological articular changes that compromise neural integrity and may influence organ system function and general health.
You may wonder, after reading my post, how the authors of the case report connected subluxations of the cervical spine to low oxygen levels in this newborn. I’ll just leave this here for your reading pleasure:
Sympathetic dominance, due to a reduced parasympathetic function or an increased sympathetic function can affect the autonomic nervous system creating a reduction in dynamic flexibility of the system, as a consequence of poor adaptation to an increase in external and internal demands. This in turn could create an imbalance in the autonomic nervous system which can have negative effects with regard to pathological conditions.
Now that is a mighty fine pseudomedical word salad, the likes of which we may not see again for many years. It’s a masterpiece of malarkey. If there were a hall of fame for this kind of thing, it definitely has my vote.
