
Anti-vaccination sentiment is highly correlated with conspiracy thinking
If you think vaccines are ineffective, you’re more likely to claim that 9/11 was an “inside job”, that Princess Diana was murdered, and that a powerful and secretive group known as the New World Order are planning to eventually rule the world. It’s also possible that you’re queasy around blood, or the thought of needles. Finally,you may be angered by anything you perceive as a limit on your freedom. If I’ve just described you, or an anti-vaccinationist you know, don’t be surprised. These correlated beliefs are not uncommon, and are the finding of a massive 24-country survey of over 5,000 adults, conducted across 24 countries. This new research provides us with a deeper understanding of what may underlie anti-vaccine ideology and perspectives, and could point the way to more effective vaccine advocacy programs.
Why can vaccines be a hard sell?
Vaccines should be as easy to sell as clean water. The risks we face in our lives today have been utterly transformed by vaccines. With the exception of clean water, no other public health measure is as effective as vaccines. Our parents and grandparents faced the risk of illness and death from diseases like smallpox, diphtheria, and polio as a fact of life. Mass vaccination completely eradicated smallpox, which used to kill one in seven children. Polio is next. Public health campaigns have also eliminated diphtheria, and reduced the incidence of pertussis, tetanus, measles, rubella and mumps dramatically. More than 100 million infants are now immunized against the most common preventable childhood illnesses each year, saving more than 2.5 million young lives each year.
Yet as long as there have been vaccinations, there have those that oppose them. Outbreaks of illnesses like measles have demonstrated that anti-vaccination sentiment is pervasive, and has real consequences. And this battle continues, even after over 100 years of immunization, and over two dozen diseases becoming vaccine-preventable.
When health professionals encounter anti-vaccine concerns or questions in their practice, the typical response may be to summarize the facts and the science, while refuting any erroneous assumptions. As a pharmacist and advocate for science-based medicine, that’s been my approach. And for some readers who are seeking a science-based perspective, that approach can be effective. Anecdotal evidence (in the form of the occasional email, or thank-you from a patient) is nice confirmation that my information help support more informed decision-making. But the negative response, particularly from those with fairly entrenched views, is more common. Moreover, it is understood, from a science communication perspective that the “explication” approach that I and others use may be ineffective: Those that may have this beliefs are not lacking in information or access to science-based sources, and may have spent a considerable amount of time gathering information to support their position. There’s some evidence of a “backfire” or “boomerang” effect where corrective information can increase, rather than decrease, perceptions about the risk of vaccines.
Motivated reasoning is thought to explain, in part, some of the ineffectiveness of traditional vaccine promotion campaigns. We may assume, as skeptics and science advocates, that evidence drives attitudes. But with motivated reasoning, the opposite is true. People develop an attitude/perspective or feeling about an issue, and then search for information to support that evolving belief. The quality of that evidence is largely irrelevant – what matters is the congruence to the initial hunch or attitude. Steven Novella highlighted this in his post yesterday, noting that through over 20 years of negative feedback, the template remains exactly the same. Those that have reached a position through motivated reasoning reject any premises or arguments that don’t align with underlying beliefs – regardless of how scientifically valid they actually are.
What this means for science advocates is that we may want to look at anti-vaccine sentiment as a symptom or manifestation of underlying attitudes and sentiments that may not have anything to directly do with vaccines. We need to understand fears, identity issues and even worldviews that lead to anti-vaccine sentiment.
The roots of anti-vaccine sentiment
So let’s take a closer look at this new study. It’s entitled “The Psychological Roots of Anti-Vaccination Attitudes: A 24-Nation Investigation” [PDF] and is from Matthew Hornsey, Emily Harris, and Kelly Fielding of the University of Queensland. It was published in Health Psychology on February 1, 2018. This is the results of an electronic survey conducted between March and May, 2016, and it probed into attitude roots that may underlie anti-vaccine sentiments. People were screened out if they were not from one of the targeted countries, were younger than 18 years of age, or if their survey responses were over 90% incomplete. This left 5,323 responses that were analyzed (about 200-300 per country). (All the supplemental materials, if you’re inclined, can be downloaded here.) Questions were written in English then translated into different languages, with adaptations to address culture-specific words and concepts. The responses to the questions above were then examined to look for relationships between questions. The attitude roots were studied:
- Conspiratorial Beliefs, with the authors choosing four that were felt to have worldwide recognition. The survey asked for agreement in conspiracy theories about:
- The assassination of President John F. Kennedy.
- The death of Princess Diana.
- The existence of a New World Order.
- The 9/11 terrorist attacks.
- Disgust, where participants rated the extent to which they would feel disgust or repugnance if they were exposed to these objects or events:
- Having blood drawn from your arm.
- Receiving an injection in the arm.
- A small vial of your blood.
- A bottle of your blood.
- Handling a hypodermic needle.
- Receiving an anaesthetic injection in the mouth.
- Reactance, which was a measure of attitudes related to communicating to others the type of person you would like to be. That is, do you communicate non-conformist ideas as part of your identity? Agreement with the following statements was evaluated:
- I find contradicting others stimulating.
- I consider advice from others to be an intrusion.
- I become angry when my freedom of choice is restricted.
- I resist the attempts of others to influence me.
- When someone forces me to do something, I feel like doing the opposite.
- Individualism – Hierarchy Worldview, to distinguish between individualistic perspectives (e.g., preferable that individuals make decisions for themselves) and hierarchicalism perspectives (hierarchies and power differences are natural and healthy) from communitarianism (where interests of communities and societies dominate over the individual) and egalitarianism (emphasizing equal rights and opportunities). The survey asked for the degree of agreement or disagreement to questions like:
- We have gone too far in pushing equal rights in this country.
- Our society would be better off if the distribution of wealth was more equal.
- We need to dramatically reduce inequalities between different groups of people in society, for example, the rich and the poor, and men and women.
- Discrimination against minorities is still a very serious problem in our society.
- It seems like many minority groups in society don’t want equal rights, they want special rights just for them.
- The government interferes far too much in our daily lives.
- Sometimes governments need to make laws that stop people from hurting themselves.
- It’s not the government’s business to try to protect people from themselves.
- The government should stop telling people how to live their lives.
- The government should do more to advance society’s goals, even if that means limiting the freedom and choices of individuals.
- Government should put limits on the choices individuals can make so they don’t get in the way of what is good for society.
- Anti-vaccination beliefs, such as agreement with the following:
- Children get more vaccinations than are good for them.
- Many of the illnesses that vaccines prevent are severe.
- It is better for my child to develop immunity by getting sick than by getting a vaccine.
- It is better for children to get fewer vaccinations all at the one time.
- Anti-vaccine sentiment was also tested based on concern expressed about the following issues:
- How concerned are you that your child might have a serious side effect from a vaccine?
- How concerned are you that any one of the childhood vaccines might not be safe?
- How concerned are you that a vaccine might not prevent the disease?
Relationships between anti-vaccination attitudes and other beliefs
The bulk of the paper, some of which I will summarize here, is an analysis of the relationships between these different questions, stratified by country. (I will leave it to our statistician readers to comment on the modelling used.) The scores on anti-vaccine attitudes were felt to be normally distributed, with 14.8% of respondents stating strong anti-vaccination attitudes, 39.2% moderately-strong anti-vaccination attitudes, 36.2% with moderately-strong pro-vaccination attitudes, and 9.8% reporting strong pro-vaccination attitudes. The strongest antivaccination attitudes skewed more towards the Asian countries, and the weakest in were in “Western” countries. The overall beliefs in the different categories are reported in Table 1:
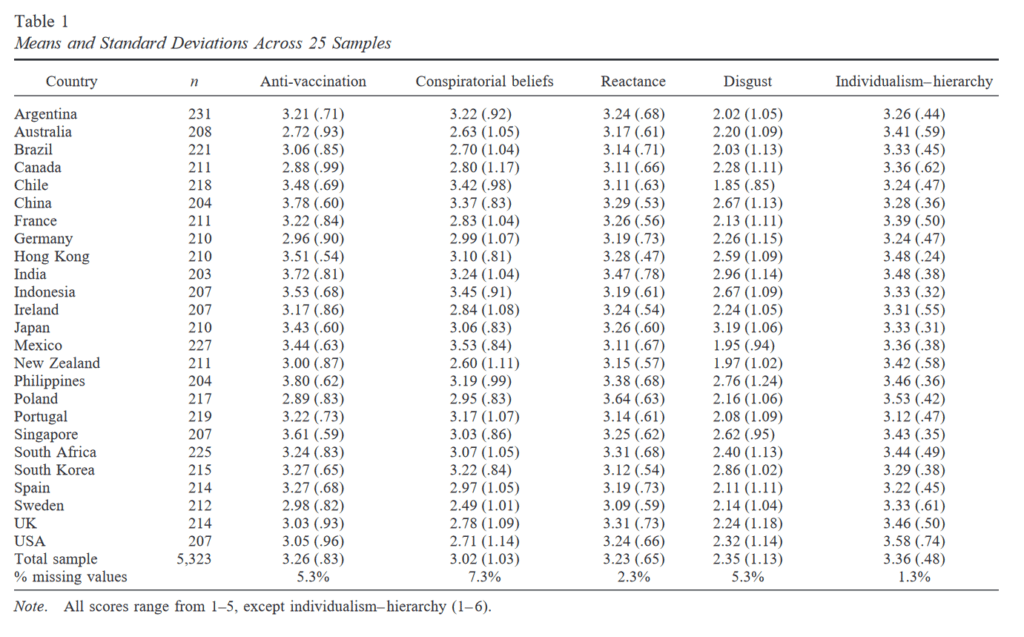
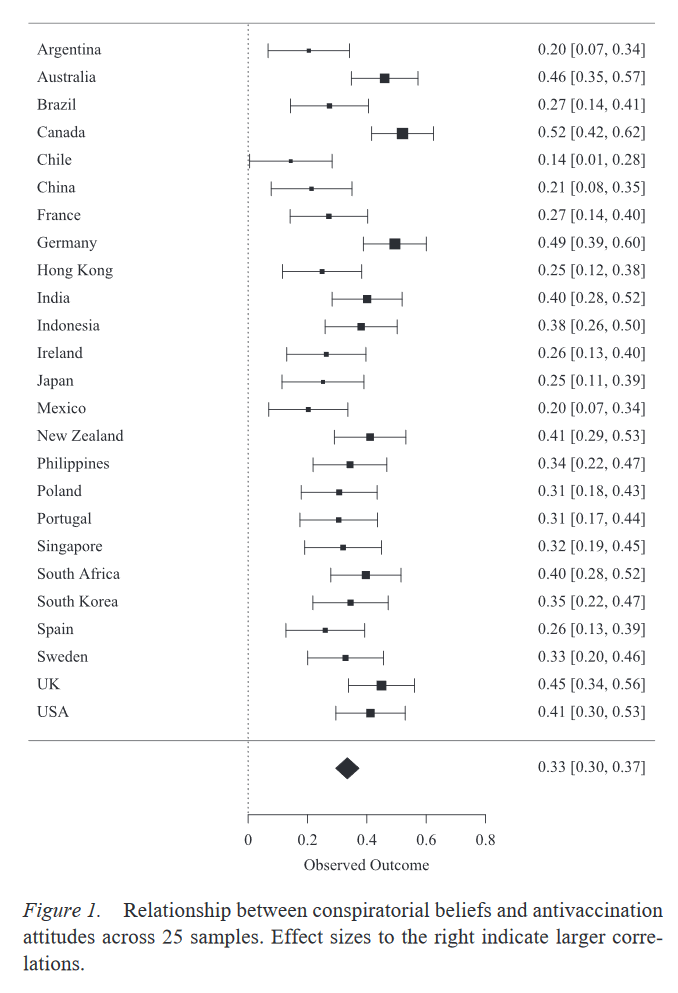
The country-level correlations are interesting. The headlines emerging from this paper noted the strong degree of correlation between anti-vaccination attitudes and conspiracy beliefs, which was observed in every country (overall r=0.33, p<0.001). The relationship between anti-vaccine sentiment and conspiracy thinking is not consistent, however. Note that China has a relatively-high reported degree of anti-vaccine sentiment in Table 1, but relatively little of this seems attributable to conspiracy theories. In Canada, in contrast, more modest anti-vaccine sentiments seems to be more closely correlated with belief in conspiracy theories.
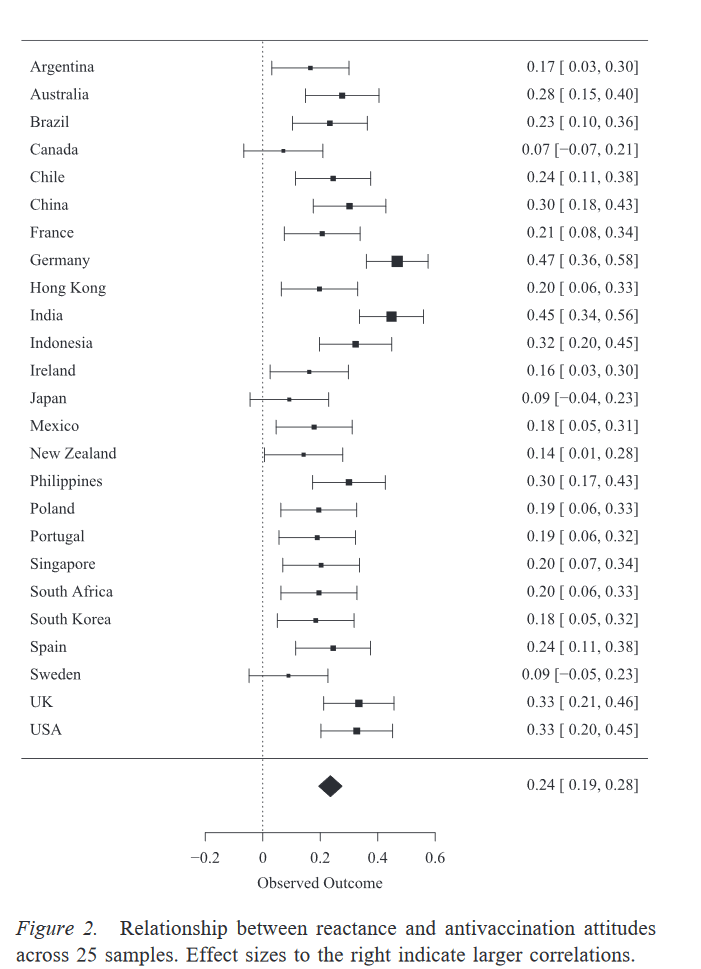
The next most consistent relationship was between reactance and anti-vaccination attitudes. The more people reported concerns about freedom of choice, or advice/influence from others, the greater correlation with anti-vaccination attitudes. Again, there are regional differences:
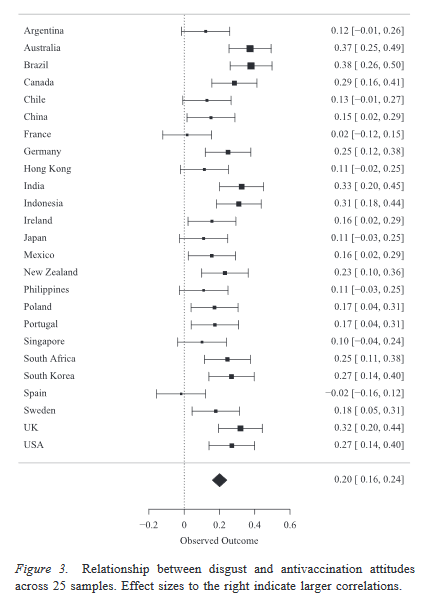
Here’s the correlation with disgust measures, which is weaker overall than reactance, but still significant in some regions:
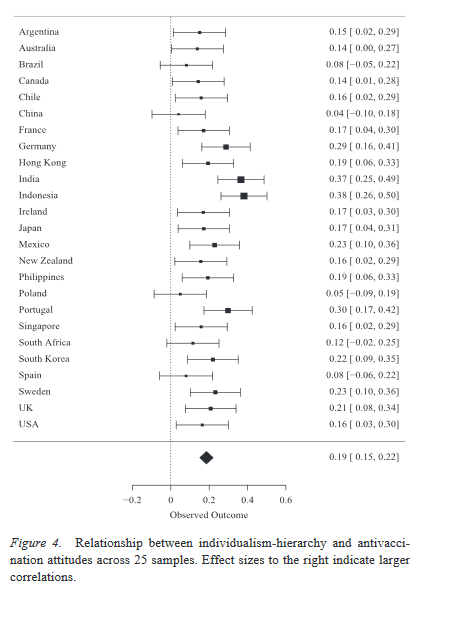
And finally, here is the correlation between anti-vaccination attitudes and individualistic/hierarchical worldviews – even less of an effect size overall, possibly because anti-vaccine sentiment can manifest based on both the Left and Right.
Antivaccination sentiment might not just be about vaccines
This study provides new information that may help to inform more effective vaccination advocacy. Importantly, the barriers to vaccines may not be the vaccines themselves – criticism of vaccines may be a manifestation of underlying perspectives or worldviews that will not be affected by straightforward science advocacy campaigns that simply state the facts. The correlations found in this paper are not consistently strong, and so they do not provide a simple complete explanation for all the reasons that individuals may hold anti-vaccine views. While the authors don’t have any “magic bullets” to solve this problem, they suggest that change may be more effective if targeted at some of these underlying motivations. For example, while reducing a conspiracy belief is admittedly difficult, the authors suggest highlighting the real possibility of vested interests on “both sides”, such as those that be motivated to downplay the benefits of vaccines, possibly to sell their own products or services. For other fears, like reactance, campaigns that show images of the real harms of preventable illnesses could potentially help individuals overcome their shorter-term anxiety about the vaccination itself. Practically speaking, what this survey may be telling us is that public campaigns may always be somewhat limited in their effectiveness. It may take focused dialogue between health professionals and their patients to understand the motivated reasoning at work, hopefully leading to more science-based attitudes about vaccines.
Reference: “The Psychological Roots of Anti-Vaccination Attitudes: A 24-Nation Investigation,” by Matthew Hornsey, PhD, Emily Harris, PhD, and Kelly Fielding, PhD, University of Queensland. Health Psychology, published Feb. 1, 2018.
Related reading:
Inoculating – Against Misinformation
What does “anti-vaccine” really mean?
>Does society try to shame and shun vaccine refusers and the vaccine-averse?
>The characteristics of antivaccine networks on Facebook
Photos from flickr users Apionid and Daniel Paquet used under a Creative Commons License.

