 I’m a breast cancer surgeon and researcher. As such, I’ve dedicated my professional career to the multidisciplinary care of women (and men) with breast cancer, using my clinical judgment and surgical skills to the best of my ability to surgically extirpate breast cancer from my patients, either before or after chemotherapy, in collaboration with medical and radiation oncologists, as well as plastic surgeons in the cases of women who require total mastectomy to eliminate their cancer. I’ve also managed to keep a lab funded for 19 years studying various aspects of breast cancer, including tumor angiogenesis and glutamate signaling. Here at Science-Based Medicine, I’ve dedicated my efforts to combatting medical myths and pseudoscientific medicine, but I do take a special interest in such misinformation about breast cancer because, well, it’s my specialty. So it was with great annoyance that I read an article I saw on Twitter late last week about Dr. Kristi Funk, who, it just so turns out, is Angelina Jolie’s breast surgeon:
I’m a breast cancer surgeon and researcher. As such, I’ve dedicated my professional career to the multidisciplinary care of women (and men) with breast cancer, using my clinical judgment and surgical skills to the best of my ability to surgically extirpate breast cancer from my patients, either before or after chemotherapy, in collaboration with medical and radiation oncologists, as well as plastic surgeons in the cases of women who require total mastectomy to eliminate their cancer. I’ve also managed to keep a lab funded for 19 years studying various aspects of breast cancer, including tumor angiogenesis and glutamate signaling. Here at Science-Based Medicine, I’ve dedicated my efforts to combatting medical myths and pseudoscientific medicine, but I do take a special interest in such misinformation about breast cancer because, well, it’s my specialty. So it was with great annoyance that I read an article I saw on Twitter late last week about Dr. Kristi Funk, who, it just so turns out, is Angelina Jolie’s breast surgeon:
Angelina Jolie’s breast surgeon explains what to eat and how to live to help avoid cancerhttps://t.co/kW3xPQNzS9
— i newspaper (@theipaper) July 29, 2018
The article to which they refer is this excerpt from her book entitled “Angelina Jolie’s breast surgeon explains what to eat and how to live to help avoid cancer.” The article reminded me that, two weeks ago, Dr. Funk had promoted a very similar message in an interview in the The Sunday Times in the UK entitled “Meet Kristi Funk, Angelina Jolie’s cancer doctor.” That’s pretty generic, but the subtitle gives away the game: “Kristi Funk is the go-to breast surgeon in Beverly Hills. She thought she knew everything about cancer risk, then she looked into diet.” I was at NECSS at the time, and therefore didn’t have a chance to write about it. By the time I remembered it again, I thought I had blown my chance and just moved on. Thankfully (well, not really) Dr. Funk has a book to promote:
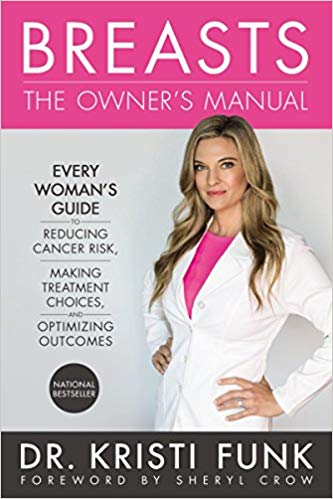
I'll be chatting about my book, "Breasts: The Owner's Manual" on @TheDoctors and live on KCal 9 News with @CBSLAsandra today. Be sure to tune in! #BreastManual https://t.co/KQkIE49J6b
— Dr. Kristi Funk (@drkristifunk) April 4, 2018
And:
It's Book #ReleaseDay. So thankful to everyone who is making this such a smashing success (you all know who you are and I love you)! Keep spreading the good word, there is a woman out there whose life will be saved as a result! #BreastManual https://t.co/Twyy0wRPsa pic.twitter.com/O3X3WagVDe
— Dr. Kristi Funk (@drkristifunk) May 2, 2018
And:
I’m so thrilled for my friend and doc @DrKristiFunk on the release of her new book, BREASTS: The Owner’s Manual! You will LOVE this book, and it will become the Breast Bible for women all over the globe. https://t.co/VqPy9MMv0V #BreastManual pic.twitter.com/leGYIVu0DB
— Sheryl Crow (@SherylCrow) April 30, 2018
And:
To keep the girls pain-free, @drkristifunk says you should first think about what you put on your plate! https://t.co/JvYeTDzPSt
— Rachael Ray Show (@RachaelRayShow) July 26, 2018
Most importantly, though, for purposes of this slew of interviews and op-eds in the UK, apparently her book was just published in the UK this month:
Today we're proud to publish this straight-talking, myth busting guide to breast health from @drkristifunk. https://t.co/g6uVTMHhdO #OutNow #NonFiction pic.twitter.com/UKbGfhGXiT
— HQ Stories (@HQstories) July 12, 2018
So obviously, Dr. Funk’s appearances in UK newspapers are part of her book promotion. Nothing wrong with that. What I do have a problem with is that Dr. Funk is promoting a message that is not well-rooted in science. Actually, that’s putting it mildly, particularly her claims about how much a woman can reduce her risk of breast cancer with lifestyle and diet interventions alone. But, first, who is Dr. Funk?
Dr. Kristi Funk: Breast cancer surgeon to the stars
I’ve mentioned Dr. Funk before in the context of discussing Angelina Jolie’s breast cancer surgery five years ago, specifically Jolie’s decision to undergo a bilateral mastectomy because she has a BRCA1 mutation. At the time, I noted that Dr. Funk founded the Pink Lotus Breast Center in Beverly Hills, where Dr. Funk has become the breast surgeon to the stars, including Sheryl Crow and Angelina Jolie. Basically, she appears to be a former academic breast surgeon who’s found a far more—shall we say?—lucrative niche taking care of wealthy and famous women in southern California. Her previous bio (no longer on the Pink Lotus website, but available through the Wayback Machine) lists an impressive set of credentials: Medical school at Stanford; residency at UC Davis, fellowship at Cedar-Sinai in Los Angeles; Director of Patient Education at the Cedars-Sinai Breast Center until 2009, when she opened her Beverly Hills office. She claims several accomplishments:
Dr. Funk graduated with distinction from Stanford University in 1991, and received her medical degree from the University of California, Davis, School of Medicine. She is also a former Oxford University scholar, and worked as a research assistant at the University of California, Los Angeles (UCLA) and Baxter Diagnostics. An outstanding investigator, Dr. Funk patented a surgical device used to increase operating room efficiency, assisted in the development of a method for the rapid detection of cytomegalovirus, and helped design an in vitro antimicrobial susceptibility test.
After surgical residency at Virginia Mason Medical Center in Seattle, WA, she completed a surgical breast fellowship at Cedars-Sinai Medical Center in 2002, where she then excelled as a surgeon and Director at the Cedars-Sinai Breast Center until 2009.
Dr. Funk’s published works have appeared in Advanced Therapy of Breast Disease, Surgical Clerkship Manual, Archives of Surgery, the Journal of Gastrointestinal Surgery and the Journal of Clinical Microbiology. As a frequent presenter, she has addressed crowds at national and international Breast Cancer conferences, multiple Los Angeles-area hospitals, the Society of Nuclear Medicine, Southwestern Surgical Congress, Pacific Northwest Vascular Society, British Esophageal Group, Seattle Surgical Society, Virginia Mason Medical Center and the American Society for Microbiology, as well as numerous community audiences.
I did a bit of PubMed perusing. I must say that her publication record in the peer-reviewed literature is quite a bit less impressive than I was led to believe by her now-defunct bio. Under her maiden name (Kristi Pado), I only found two articles. I did find an article in the Archives of Surgery and in the Journal of Clinical Microbiology. She was not first or last author on either. (First author indicates the most intellectual involvement and doing most of the work, while last author usually indicates the senior author in whose lab or under whose supervision the work was carried out.) Neither had anything to do with breast cancer. Both occurred in the 1990s, when Dr. Funk was still a trainee, either as a resident or a fellow. Looking under Dr. Funk’s current name, I found one paper reporting a multicenter evaluation of a new surgical guidance technology for localizing non-palpable breast lesions. Clearly the Pink Lotus Breast Center was just one of fourteen sites where the new technology was tested. This is no big deal. Lots of clinicians agree to be site principal investigators for tests of new surgical technologies. Let’s just put it this way. Three publications in the peer-reviewed literature indexed in PubMed over 24 years, none of them first author, do not impress me that much. Other than her participation in a multicenter evaluation of a new product, she’s published nothing in the peer-reviewed literature since 1997.
As for her patents, searching for “Pado” in the inventor name column brought up 14 patents, none of them with her name. Searching with “Funk” as the name brought up 1,226 patents. Narrowing it down to Kristi Funk brought up no hits. So either she’s…mistaken…or I don’t know how to search the patent database very well. Either way, color me unimpressed—either with me or with Dr. Funk. Take your pick. If I manage to discover what her patent was, I’ll update this paragraph and give myself 100 lashes with a wet noodle for not having found it.
One thing that I did mention when I discussed Angelina Jolie’s surgery is that Dr. Funk is also enamored of “integrative medicine”. Indeed, it’s something promoted and offered by Pink Lotus, whose website proclaims that “integrative medicine is not just a marketing slogan but rather the essence of what we practice” and that “holistic medicine” is one of its services. Angelina Jolie appears to have undergone a mixture of the science-based (bilateral prophylactic mastectomy for risk reduction due to BRCA1 mutations) tinged with pure pseudoscience, like the use of homeopathic remedies such as Arnica Forte (which consists of Arnica Montana 30x, Bromelain, Antioxidants, and Bioflavonoids) as a means of decreasing bruising during surgery. Steve Novella recently wrote about how the use of homeopathic Arnica is pure quackery, with no evidence to support it, although he apparently didn’t know at the time that Dr. Funk used it on Jolie. Dr. Funk also used Exchem and Lymphomyosot (“to help eliminate anesthesia from the system”) when operating on Jolie. So, yes, Dr. Funk recommends “detox,” which is the purpose for which Lymphomysot is advertised, to get rid of anesthesia agents after surgery.
To sum up thus far, Dr. Funk was at one time on the academic surgery track but hasn’t done any significant research in decades and her publication record is not impressive. She was involved in education for a long time at Cedars-Sinai, but she left that behind ten years ago when she went private and founded Pink Lotus Breast Center. Since then, she’s been heavily into “holistic” treatments mixed with standard breast cancer surgery, mixing the sensible and science-based with exaggerated claims for the effects of diet on breast cancer risk and pure woo like homeopathy during surgery. Thanks to her success in attracting Hollywood glitterati as her patients, she’s become rather famous and is frequently seen on TV and in the media. Now she’s written a book, whose UK launch was accompanied by a lot of her misinformation. So what are we talking about?
The Clones of Dr. Funkenstein: Dr. Kristi Funk versus breast cancer genetic risk factors
Dr. Funk’s tweets were met with a strongly critical response by Dr. Liz O’Riordan, a British breast surgeon who has herself been diagnosed with recurrent breast cancer. In this section, I basically explain why Dr. O’Riordan’s criticisms are correct. (I know, I know, she’s a surgeon in the UK; I don’t care, given that I’m in the US right now.) Here’s what she says:
WTF? This woman claims that if you are tall or eat cheese or any meat you will get breast cancer. SCARY and WRONG! https://t.co/RMMzLf9OkS
— Dr Miss Dr Mrs Liz O'Riordan (@Liz_ORiordan) July 12, 2018
And:
WTF? “80% of all breast cancer could be eliminated from planet Earth if women understood that daily choices eg food, drink, and mindset create the environment inside the cells of our breasts, which turn malignant” @Independent this is DANGEROUS and WRONG! https://t.co/FpTF2lo0uM
— Dr Miss Dr Mrs Liz O'Riordan (@Liz_ORiordan) July 28, 2018
If the interviews she’s done and the articles she’s published are any indication, the key message that Dr. Funk appears to be promoting in her book, Breasts: The Owner’s Manual: Every Woman’s Guide To Reducing Cancer Risk, Making Treatment Choices, And Optimizing Outcomes, is one of control. For example, take a look at this most recent article in the UK’s inews:
One big problem with breast cancer awareness is erroneous public perception.
Most women believe that family history and genetics determine who gets breast cancer – but 87 per cent of women diagnosed do not have a close relative with the disease.
On the other hand, research really does tell us that if women embrace a lifestyle, before reaching menopause, that prioritises exercise, not smoking, not drinking alcohol, and a diet shifted away from meat and dairy toward whole-food, plant-based eating, their odds of getting breast cancer are slashed in half. And for older women, risk drops by 80 per cent.
One of the most dangerous falsehoods is that your diet doesn’t impact breast health, which is completely wrong. What you put into your body influences oestrogen levels – which fuel 80 per cent of all breast cancers – as well as inflammation, blood vessel formation, cellular function, and destructive free radicals, to name a few cancer-related factors.
One can see why Dr. Funk’s message is so appealing. She’s basically telling women that they can reduce their risk of breast cancer by 80%! In her interview in The Sunday Times, she was even more blunt:
When polled, most say that breast cancer is down to genetics, when in fact 87 per cent of women diagnosed do not have an immediate relative with the disease. Funk says that up to 90 per cent of the risk factors for the disease lie in our control, “not your doctor’s, genes or fate”. Funk assumed that they were the usual commandments to exercise and avoid chub and alcohol, but she was surprised to see study after study proving how much diet plays a role.
What is the biggest lifestyle risk factor for breast cancer? “Definitely nutrition. Then obesity, alcohol, exercise, hormone replacement therapy, stress.”
Unfortunately, Dr. Funk’s “logic” is based on a faulty understanding of genetics and risk. Nowhere could I find a better example of that than in an excerpt from her book that was published in Kevin, M.D., entitled, “Debunking breast cancer myths: the truth about genes, gender, and destiny.” (By the way, WTF are you doing publishing this rot, Dr. Pho? Seriously, your blog has gone way, way downhill!) Get a load of the first passage:
Genetics play a less important role than you probably think. Consider this fact: the identical twin sister of a woman with breast cancer has only a 20 percent chance of getting breast cancer one day—which, by the way, is the same risk as anyone with an affected sister. Since these twins share the exact same DNA, if genetics called all the cancer shots, risk should approach 100 percent—but it doesn’t, because genes aren’t the be-all end-all many people think they are.
Patient after patient tells me that there isn’t any breast cancer in her family, so she’s not really at risk. Yet 87 percent of women diagnosed with breast cancer do not have a single first-degree relative with breast cancer. In fact, only 5 to 10 percent of breast cancers currently prove to be hereditary, meaning that they occur because abnormal gene mutations pass from parent to child.
I sense a thousand geneticists out there grinding their teeth in unison at these statements. I know that she’s trying to counter a myth that breast cancer is entirely genetic in nature, but in doing so she goes way, way too far in the other direction. She assumes that just because only around 5-10% of breast cancers have a mutation in a known cancer-causing gene (like Angelina Jolie did in BRCA1) and only 13% of patients have a first-degree relative with breast cancer that genetics is much less important than sold and that 87% of breast cancer cases are potentially preventable. This is rubbish of the highest order. For one thing, increased risk due to relatives with breast cancer is more complex than that. More importantly, though, it’s “dose-dependent”. For instance, one first degree relative with breast cancer roughly doubles a woman’s risk, but if she has more than one first degree relative her risk is three- to four-fold higher. Age at diagnosis matters, too. The younger a first-degree relative is diagnosed with breast cancer, the more it matters, particularly before age 40. These are all indications of a genetic predisposition. I will give Dr. Funk credit for mentioning that the male side of the family matters, but her assumption that 80% or more of breast cancer can be prevented is not well-supported by evidence. And, make no mistake, she does make exactly this claim in her book (about 50 pages of which are available as an excerpt on Google Books), claiming that if you do what she says and exercise, don’t drink alcohol, don’t smoke, and shift your diet away from meat and dairy towards “whole food” plant-based eating before menopause you will slash your postmenopausal risk of breast cancer by 80% (p. 14).
I can’t help but note that the most potent known breast cancer-causing mutations in the BRCA1 gene only result in a roughly 80% lifetime risk of breast cancer, which is around seven times higher than that of the average woman.
The Clones of Dr. Funkenstein: Dr. Kristi Funk vs. lifestyle-based risk factors for breast cancer
It’s kind of depressing to read several of the articles by Dr. Funk and interviews with her, because you quite regularly see her saying that you must give up meat and dairy because they “fuel” breast cancer. She does it in hyperbolic terms, as well, citing the aforementioned claim that you can decrease your risk of breast cancer by up to 80%. Indeed, in the Sunday Times article, she even laid the fear on the journalist doing the article, Helen Rumbelow, by scaring her about her daughter’s love of dairy:
After this, my mind wanders to my adolescent daughter, who likes to drink a glass of full-fat milk a day because the evidence shows that this boosts height. A preliminary study by Michigan State University showed that a high-saturated fat diet in puberty sped up breast cancer in adult women.
“If she drinks milk she will grow because her body’s response to that is to spike her insulin-like growth factor, but she will also be setting the stage for illness. So I’d rather her be a little shorter,” says Funk.
Given that I’m in Michigan, I was really curious what this study was. I couldn’t find it in her book excerpts, and I couldn’t find it in any of her articles or interviews. So, I Googled, with not a lot of hope of finding the study. Find it, I did, though, through a press release by MSU. I call foul. Notice how Dr. Funk refers to this as a preliminary study. That is true, but in actuality it is a preclinical study in that it was a study done in mice! Worse, this was a mouse study where prepubertal mice were fed a low fat or high fat diet and then subjected to a chemical mutagen to induce mammary carcinogenesis. In other words, it’s a highly artificial model. While it’s an interesting result, whether or not it has anything to do with human puberty is less than a coin toss in likelihood. While mouse mammary development has been a useful model, there are many differences between human and mouse mammary glands. I’m guessing that SBM readers can see why such a study might not tell us much about the situation in humans.
What is the evidence regarding dairy as a breast cancer risk in humans? Let’s just say that it’s quite a bit less…impressive…than Dr. Funk seems to think. In fact, it’s largely negative or at the very least controversial and highly questionable. For instance, a study published just this year found “no overall association between dairy consumption during adolescence or early adulthood and breast cancer risk” and that dairy consumption during adolescence “may not be a significant predictor of breast cancer incidence.” (My reading of the study is that it was negative.) Indeed, a meta-analysis of prospective cohort studies published in 2011 suggests that “increased consumption of total dairy food, but not milk, may be associated with a reduced risk of breast cancer.” (That’s cheese and other dairy products they’re talking about.) That’s not the only one. A study from 2002 found decreased risk associated with dairy intake. Meanwhile another study found results “not supportive of a positive independent association between consumption of animal fat and breast cancer, although findings may be sensitive to the type of dietary instrument used in cohort studies.” A study from Roswell Park found no significant association between total dairy consumption and breast cancer risk but noted a positive association between milk consumption and certain subtypes of breast cancers. Finally, a 2004 meta-analysis concluded that “available epidemiologic evidence does not support a strong association between the consumption of milk or other dairy products and breast cancer risk.” In other words, it’s complicated. Several major studies consistently found lower risk associated with total dairy intake, but some found higher risk of certain subtypes of breast cancer associated with certain types of dairy. Basically, if dairy consumption does increase breast cancer risk (and my reading of the current literature is that it probably does not), the effect size is almost certainly quite small, at the limits of detection in epidemiological studies.
But what about meat? Dr. Funk makes it sound as though meat, especially processed meat, is a deadly breast cancer-inducing food that women should avoid like the plague. There might be something there, but, again, Dr. Funk appears to be vastly exaggerating the increased risk attributable to meat consumption. For example, a study from this year found an odds ratio for breast cancer of 1.16 among women with the highest consumption of processed meat. A recent British cohort study and meta-analysis found a relative risk of 1.21 among the highest tertile of processed meat consumption. However, when combined with ten previous cohort studies, the relative risk fell to 1.06 overall. That broke down to no association between processed meat consumption and breast cancer in premenopausal women and a relative risk of 1.09 in postmenopausal women. We’re talking single digit increases in risk here. As for red meat, there was no correlation. An earlier review and meta-analysis concluded that “red meat and processed meat intake does not appear to be independently associated with increasing the risk of breast cancer.” I could go on, but you get the idea.
Basically, Dr. Funk appears to have cherry picked studies finding the largest associations, while ignoring the mass of epidemiological evidence that came to conclusions she doesn’t like, such as:
- Although there might be a small increased risk due to high consumption of processed meat (but not red meat), it’s only among those consuming the most. There is no good rationale, based on these studies, to give up meat as a means of dramatically reducing breast cancer risk.
- The epidemiological data regarding dairy consumption and breast cancer risk is noisy, but is fairly clear that there probably isn’t an increased risk attributable to overall dairy consumption—and might even be a decreased risk. There might be a modest increase attributable to specific kinds of dairy products for specific subtypes of breast cancer, but my reading of this data is that the data are dicey and not very strong evidence for an association. That means that there is no good scientific basis for recommending eliminating dairy as a strategy to dramatically reduce one’s risk of breast cancer.
That’s about it. Basically, Dr. Funk makes a lot of claims that aren’t supported by science.
Dr. Funk oversells vegan diets
But what about vegan diet as a means of decreasing breast cancer risk? One message that Angelina Jolie appears to have imbibed from Dr. Funk is that going vegan will radically reduce her risk of recurrence and, among women who have never had breast cancer, greatly reduce the risk of it in the first place. Here’s what Dr. Funk claims:
The studies on vegans and breast cancer risk are, she concedes, somewhat muddy. The numbers of vegans have just been too low in the West, although it is worth noting that populations with low breast cancer rates typically eat little meat or dairy. The largest study on vegans and breast cancer is the Adventist Health Study, in which vegans (as opposed to vegetarians) showed a 44 per cent drop in breast cancer rates compared with meat eaters, or, as the researchers wrote in the journal Cancer Epidemiology, “vegan diet seems to confer lower risk for . . . female-specific cancer than other dietary patterns”.
Funk is confident that future studies will prove more conclusive because of other research done on the effects of animal fat and protein. Essentially, this is where the hormones and “growth factors” that make westerners so big, tall and possibly cancerous are stored. So, in the case of dairy, studies show no breast cancer risk of consuming low fat.
Actually, the studies don’t show much (if any at all) risk due to high fat dairy either. Be that as it may, Dr. Funk is really reaching here. She’s correct that there isn’t a lot of strong evidence. For instance, this study suggest that a vegan diets can modestly decrease total cancer risk, but the relative risk was only 0.92 (an 8% risk reduction). As for the Adventist Health Study (AHS), I can’t help but note a couple of things. First, it doesn’t seem to matter much what kind of vegetarian one is in terms of all-cause mortality, which is what really matters: The adjusted hazard ratio (HR) for all-cause mortality in all vegetarians combined vs non-vegetarians was 0.88 (95% CI, 0.80–0.97). The adjusted HR for all-cause mortality in vegans was 0.85 (95% CI, 0.73–1.01); in lacto-ovo–vegetarians, 0.91 (95% CI, 0.82–1.00); in pesco-vegetarians, 0.81 (95% CI, 0.69–0.94); and in semi-vegetarians, 0.92 (95% CI, 0.75–1.13) compared with nonvegetarians. Those numbers are all pretty similar; so I want to keep eating my fish, dairy, and eggs. Second, as for the risk of breast cancer, I’m confused. The latest publication from the AHS I could find was from 2016, and its findings were not nearly as striking as what Dr. Funk reports:
As compared with non-vegetarians, all vegetarians combined did not have a significantly lower risk (hazard ratio (HR) 0·97; CI 0·84, 1·11; P=0·64). However, vegans showed consistently lower (but non-significant) point estimates when compared with non-vegetarians (all cases: HR 0·78; CI 0·58, 1·05; P=0·09). In summary, participants in this cohort who follow a vegetarian dietary pattern did not experience a lower risk of BC as compared with non-vegetarians, although lower risk in vegans is possible. These findings add to the very limited literature associating vegetarian diets with BC risk and can assist nutritionists when evaluating the impact of these diets. The findings will also motivate further evaluation of vegan diets and their special characteristics.
Going back through the publications based on the AHS (and there are many), I think I found what happened. The most generous conclusion is that Dr. Funk confused studies. The publication that she cited to Rumblelow reported a decreased risk of female-associated cancers (breast, ovarian, endometrial), with a relative risk of 0.66, and included the exact same phrase (taking the ellipse into account) that Dr. Funk had provided in her article (“vegan diet seems to confer lower risk for overall and female-specific cancer compared to other dietary patterns”). Of course, she cited a 44% decreased risk, and this study found a 34% decreased risk, but I suspect she just had a brain fart and made a mistake in mental subtraction. (Again, that’s the most generous interpretation.) What can’t be reconciled is the claim that a vegan diet decreased the risk of breast cancer by 44% in the AHS and the actual evidence. The study cited does not show that, because breast cancer wasn’t broken out from “female-associated cancers”. A more recent publication (but still not so recent that she shouldn’t have been aware of it before the publication of her book), the very study that Dr. Funk cited, failed to find that a vegan diet confers a lower risk of breast cancer compared to a non-vegan diet. It found that a vegan diet might confer lower risk. Might. That’s a heck of a lot less definitive than the message that Dr. Funk is promoting, which is that meat and dairy are killing women by giving them breast cancer.
Finally, there is the issue of obesity. Obesity is definitely a risk factor for breast cancer. This has been known for a while. The relative risk varies among studies, but in general the risk is highest in postmenopausal women and for estrogen receptor-positive tumors, and can be as high as a relative risk of 1.7. So maintaining a healthy weight is indeed one way to decrease one’s risk of breast cancer. However, Dr. Funk comes across as borderline victim-shaming in discussing this. I’m not the only one who thinks so. Here’s the thing, though. Being obese, no matter how a woman got there, is probably the single most potent non-genetic lifestyle-based risk for breast cancer. Given that vegans tend to be slimmer, I find it interesting that the available evidence shows that a vegan diet probably doesn’t decrease a woman’s risk of breast cancer.
Alcohol: The cause of and solution to all the world’s problems
Dr. Funk is correct when she points out that alcohol increases the risk of breast cancer. However, the effect size is relatively modest, although it is dose-dependent. Cancer Research UK has a handy-dandy infographic that tells the story. For under three units a day, the additional risk is less than 5%, but it rapidly rises between 3-6 units/day and for >6 units/day. In other words, unless you’re a heavy drinker, the added risk from alcohol consumption is small.
Here’s where Dr. Funk goes from crystal clarity (“it is crystal clear that the body’s cellular response to animal protein and fat is nothing but dangerous“) to downright fuzzy, in inverse relation to the fuzziness of the evidence. The data with respect to meat and dairy as risk factors for breast cancer range from negative to only suggestive. Yet Dr. Funk is near-absolutist telling women not to eat dairy or meat, portraying them as full of inflammation-causing, cancer-inducing poisons whose elimination will dramatically decrease a woman’s risk of breast cancer. In direct contrast, there is no doubt in the literature (and hasn’t been for at least two decades) that alcohol significantly increases the risk of breast cancer in a dose-dependent fashion. Yet with alcohol she waffles. Here’s her take:
She is not unrealistic. Yes, any alcohol consumption increases breast cancer risk, but because of alcohol’s heart-healthy benefits she compromises on about one glass a day — and studies suggest that red wine may be the least damaging to breasts. Also, you know that thing people do when they eat a big salad to “trade off” their drink? It’s not ridiculous, it actually works. In the Nurses’ Health Study, among those drinking at least one glass of wine a day, those who also ate a few servings of green vegetables (adding up to 600 micrograms of folate) had 89 per cent less breast cancer than drinkers who did not.
This is rationalization at its finest. Dr. Funk likes wine; so she finds a reason why she can have a glass of wine every day. She’s not unreasonable, either. Everything is balancing risks and benefits in medicine, including diet. Yet she doesn’t apply the same reasonableness to meat, dairy, and all the other evil (to her) things that she views as breast cancer-causing killers. She also overestimates the evidence again, to allow her to rationalize her glass of wine a day. It’s not nearly as clear as she makes it that a daily glass of wine is heart-healthy. The issue is still fairly controversial.
Putting it all in perspective
Unfortunately, along with the sensible advice for decreasing breast cancer risk (lose weight; don’t smoke; exercise), Dr. Funk is selling a lot of dubious advice too (vegan diets, no meat, no dairy). It goes even beyond what I’ve discussed thus far. Apparently, earlier this year in an interview with Good Morning America, she suggested interventions like eating more cruciferous vegetables, antioxidant-rich berries, turmeric, Indian Gooseberry, mushrooms, and soy. Let’s just say that the evidence that any of these foods decrease the risk of breast cancer is slim to nonexistent. Perhaps the most bizarre advice she gave was to use bar soap instead of antibacterial soap to lower the risk of exposure to “toxins”. Again, this is basically nonsense, as was her advice to fill your home with houseplants to “absorb toxins”. Indeed, her message is so muddled and without support that a group of surgeons in the UK wrote a letter to The Sunday Times:
The Times published a shocking article from Dr Kristi Funk saying women were responsible for getting breast cancer – they shouldn't be tall or eat cheese or meat… This is the response from a group of senior Drs with cancer – they cut the letter but you get the point… pic.twitter.com/F4E045Xj0a
— Dr Miss Dr Mrs Liz O'Riordan (@Liz_ORiordan) July 17, 2018
Finally, above all Dr. Funk’s message is one of control. While it’s good to give patients a sense of control over their destiny, it does them no service to give them such an exaggerated sense of control wherein she tells them that they can reduce their risk of breast cancer by 80% when the evidence does not support that. Therein lies the path to blaming the victim. Contrary to what she claims, many of the risk factors for breast cancer are outside of a woman’s control. That doesn’t mean that there aren’t things a woman can do to significantly decrease her risk, such as losing weight, exercising, and not drinking to excess. (Believe it or not, smoking is not a strong risk factor for breast cancer, although it’s still a good idea not to smoke because obviously smoking is a strong risk factor for lung and several other cancers, as well as cardiovascular and lung disease.) However, there will always remain factors beyond her control. For example, the two strongest risk factors are female sex and age. Most cases of breast cancer are diagnosed over age 55 (median age 62). Other factor are family history, age at menarche and menopause, and the like. Others are, strictly speaking, controllable, but not really that practical to control. After all, who’s going to have a child at a young age to decrease her risk of breast cancer? Who’s going to have a lot of children just to reduce her risk of breast cancer? These are, of course, risk factors that have been known for a long time.
The bottom line is that evidence-based recommendations for how to reduce breast cancer risk are not sexy. Lose weight. Exercise. Don’t drink too much. Boring! That sort of advice doesn’t sell books, and it sure as heck doesn’t make one feel special or superior for having the will to radically change her life by giving up meat, dairy, and becoming a vegan who eats only “whole, plant-based foods,” which basically means no oils, no extracts, no vegan baking, no nothing. That’s what Dr. Funk is really selling.

