Women looking for relief from hot flashes will be disappointed if they think acupuncture will help them.
Arguably, one of the most popular forms of so-called “complementary and alternative medicine” (CAM) being “integrated” with real medicine by those who label their specialty “integrative medicine” is acupuncture. It’s particularly popular in academic medical centers as a subject of what I like to refer to as “quackademic medicine“; that is, the study of pseudoscience and quackery as though it were real medicine. Consider this. It’s very difficult to find academic medical centers that will proclaim that they offer, for example, The One Quackery To Rule Them All (homeopathy). True, a lot of integrative medicine programs at academic medical centers do offer homeopathy. They just don’t do it directly or mention it on their websites. Instead, they offer naturopathy, and, as I’ve discussed several times, homeopathy is an integral—nay, required—part of naturopathy. (After graduation from naturopathy school, freshly minted naturopaths are even tested on homeopathy when they take the NPLEX, the naturopathic licensing examination.) Personally, I find this unwillingness of academic medical centers that offer naturopathy to admit to offering homeopathy somewhat promising, as it tells me that even at quackademic medical centers there are still CAM modalities too quacky for them to want to be openly associated with. That optimism rapidly fades when I contemplate what a hodge-podge of quackery naturopathy is and how many academic integrative medicine programs offer it.
If you believe acupuncturists, acupuncture can be used to treat almost anything. Anyone with a reasonable grasp of critical thinking should recognize that a claim that an intervention, whatever it is, can treat many unrelated disorders is a huge red flag that that intervention is almost certainly not science-based and is probably quackery. So it is with acupuncture; yet, that hasn’t stopped the doyens of integrative medicine at the most respected medical schools from being seduced by the mysticism of acupuncture and studying it. I can’t entirely blame them. I must admit, there was a time when even I thought that there might be something to acupuncture. After all, unlike so many other CAM interventions, acupuncture involved doing something physical, inserting actual needles into the body. However, as I critically examined more and more acupuncture studies, I eventually came to agree with David Colquhoun and Steve Novella that acupuncture is nothing more than a “theatrical placebo.”
As I’ve said before, if you look at the evidence for acupuncture critically and in its totality, acupuncture has no specific effects and no effects distinguishable from placebo. Indeed, it doesn’t matter where the needles are inserted, in “real” or “sham” acupuncture points, or even if the needles are actually inserted in the skin (a point that will become important later in this post). It’s all the same. Basically, acupuncture is the gateway drug of “complementary and alternative medicine” (CAM) that is often a harbinger of the harder stuff, like naturopathy and homeopathy. But, if you believe its adherents, acupuncture can work for practically any symptom caused by pretty much any condition.
Acupuncture and menopause
One of the most popular uses for acupuncture is to treat menopausal symptoms. I’m familiar with this literature because the anti-estrogen drugs used to treat hormone-responsive breast cancer nearly always produce menopausal symptoms, and it is these symptoms that all too often hurt patient compliance with treatment and sometimes even lead patients to discontinue the drugs. Indeed, among practitioners of “integrative medicine” (the art of integrating quackery with real medicine), there’s a great deal of enthusiasm for acupuncture for menopausal symptoms, particularly hot flashes, which can be very troublesome for both women undergoing natural menopause and even more so for women experiencing medication-induced menopause as part of their breast cancer treatment. Worse, in the case of cancer treatment, oncologists can’t use supplemental estrogen to treat them, hence the search for other treatments. Never mind that clinical studies have been consistently unimpressive. None of this, however, prevents acupuncture advocates from continuing to do clinical trials. In fact, in just the first quarter of 2016, there have already been published two major studies examining acupuncture as an intervention to relieve menopausal symptoms. They are studies that support what we at Science-Based Medicine (SBM) have been saying all along: The more rigorous the study, the more likely it is to find no specific effect greater than that of placebo.
Acupuncture and menopause: Acupuncture doesn’t work
The first study I’ll examine was carried out in Australia. It is a perfect example of what Harriet Hall likes to refer to as “Tooth Fairy science.” To paraphrase Harriet, Tooth Fairy Science is science that studies a phenomenon that doesn’t exist. You can do studies on the Tooth Fairy comparing how much money she leaves for kids in different socioeconomic groups. You can do studies on the memory of homeopathic water. You can do studies on the therapeutic effects of manipulating imaginary human energy fields with therapeutic touch. The problem is that the phenomena under study haven’t yet been shown to exist; so Tooth Fairy science is, in essence, putting the cart before the horse. Prove the phenomenon exists before doing studies of it; this is particularly important in human trials, because doing human subjects research without having first developed a robust preclinical science base for the intervention to be studied is considered unethical—and rightly so.
No one, for instance, has ever shown that human life “energy” (qi) exists, much less that sticking little needles into the pathways in the body through which the qi flows (acupuncture meridians) can unblock or redirect the flow of qi for healing effect, nor has anyone ever shown that meridians even exist. Unfortunately, the authors the Australian study recently published in the Annals of Internal Medicine by Carolyn Ee and investigators from Melbourne Medical School, the University of Melbourne; the Royal Melbourne Institute of Technology University; Southern Cross University; Queen’s University in Ontario; and Monash Health in Clayton, Victoria, Australia seem aware of that, as you will see. It is a randomized clinical trial of acupuncture for hot flashes that occur during normal menopause entitled “Acupuncture for Menopausal Hot Flashes: A Randomized Trial.” Although there is much to admire about this trial, even with a pretty rigorous clinical trial design the authors couldn’t resist bringing traditional Chinese medicine mysticism into the mix.
This trial enrolled women older than 40 in the late menopausal transition or postmenopause with at least seven moderate hot flashes daily. Hilariously (I have to laugh so that I don’t cry) the authors further note that these women thus met the criteria for traditional Chinese medicine diagnosis of kidney yin deficiency. Curious just what “kidney yin deficiency” is, I looked it up. Here’s a description. First of all, kidney yin is:
When The [sic] theory of yin and yang is used to explain the organic structure of the human body; the physical form pertains to yin, while activities or functions pertain to yang. The physical forms are the material basis for functions, while functions are the motivating power for physical forms. They are mutually complementary. TCM views the kidneys as the center of the body’s yin and yang, the “congenital foundation,” or the origin of life. In other words, the kidneys store the primordial yin and primordial yang (also called kidney yin and yang), which is the place where nutrients are stored and physiological functions take place.
Kidney yin, also called primordial yin, true yin or true water, is the foundation of the yin fluid of the whole body; it moistens and nourishes the organs and tissues.
TCM kidneys Kidney yang, also called primordial yang, true yang or true fire, is the foundation of the yang qi of the whole body; it warms and promotes the functions of the organs and tissues.
This is, of course, utterly unscientific, based as it is on concepts not at all unlike the concepts behind “traditional Western medicine,” namely the idea that “imbalances” in something are the cause of all disease. In the case of traditional Western medicine, it’s an imbalance in the four humors. In traditional Chinese medicine, it’s an imbalance in the five elements. In any case, what are the symptoms of kidney yin deficiency? Not surprisingly, some of them resemble menopause:
Presentations of kidney yin deficiency include: soreness and weakness of the lumbar regions and knees, dizziness, ringing in the ears, hearing problems, a dry mouth and throat, a hot sensation in the palms, soles and chest, spontaneous sweating, constipation, and seminal emission. The pulse is weak or fine and rapid; the tongue is red and covered with a light coating of fur. Kidney yin deficiency syndrome always produces signs of yin vacuity internal heat.
Now, here’s where kidney yin deficiency comes into the trial, according to Ee et al:
Women were included if they were postmenopausal (>12 months since their final menstrual period) or in the late menopausal transition (follicular-stimulating hormone level ≥25 IU, amenorrhea ≥60 days, and VMSs), had a mean HF score of at least 14 (equal to 7 moderate VMSs daily) (16), or had kidney yin deficiency diagnosed using a structured Chinese medicine history as well as a tongue and pulse examination performed by experienced acupuncturists (Appendix Figures 1 and 2). Kidney yin deficiency, of which night sweats is a cardinal symptom, is a Chinese medicine clinical syndrome diagnosed in 76% to 81% of symptomatic postmenopausal women (17, 18).
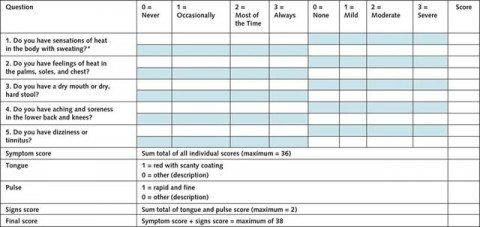
They were even kind enough to provide a questionnaire to diagnose kidney yin deficiency (click to embiggen):
As you can see, this questionnaire is so vague as to be pointless. Certainly, it’s not enough to diagnose menopause. After all, there are no questions about frequency of menstrual periods or when the subject’s last menstrual period was, and the questionnaire includes information about Chinese pulse diagnosis, which is not reproducible, and Chinese tongue diagnosis, which is basically reflexology on the tongue.
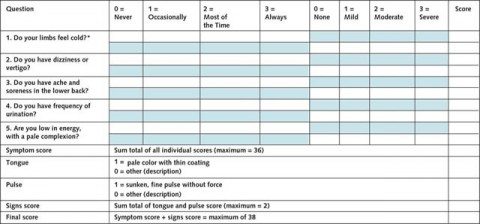
The women were also assessed for kidney yang deficiency. (I kid you not.) Kidney yang deficiency involves sore and/or weak back/knees, sensation of cold, aversion to cold, weak lower limbs, lassitude, clear copious urine, poor appetite, loose stools, edema (which can be severe). Here’s the questionnaire Ee et al used (click to embiggen):
According to the paper, the final scores for kidney yin and yang deficiency were compared, and women who scored higher for kidney yin deficiency were eligible for the trial.
So far, not so good. If only the authors had stuck to standard “Western” medical definitions of menopause, instead of bringing in prescientific mystical beliefs of traditional Chinese medicine.
Leaving aside the study’s inclusion and exclusion criterial, I note that 327 women were randomly assigned to acupuncture (n=163) or sham acupuncture (n=164). The study was blinded, but not completely. Study design was a stratified, blind (participants, outcome assessors, and investigators, but not treating acupuncturists), parallel, randomized, sham-controlled trial with equal allocation. Overall, it wasn’t a bad design as far as acupuncture studies go. Its main defect is that the treating acupuncturists were not blinded, which would have been required for a true double-blind study design, but other than that the study did use a pretty good acupuncture sham, the Park-style fake retractable needles that don’t break the skin, which were also inserted in the “wrong” places. In any case, participants received 20 minute acupuncture sessions (or sham acupuncture sessions) twice weekly for two weeks and then weekly thereafter.
So what were the results? Do you even have to ask? Basically, this was a completely negative trial, which is why I wasn’t as concerned about whether or not the acupuncturists were blinded or not. (This would have been a much bigger issue if there had been a positive result.) At the end of the eight week treatment period, mean hot flash scores were 15.36 in the acupuncture group and 15.04 in the sham group (P=0.77). Hot flash scores declined about 40% in both groups and persisted for six months. The investigators couldn’t find evidence of an advantage of acupuncture over sham acupuncture on quality of life, anxiety, or depression. That’s about as negative as it gets. I do have to give the investigators credit. They didn’t try too hard to torture the data to provide the result they wanted with post hoc analyses, as many investigators carrying out clinical trials of CAM (and, let’s admit it, non-CAM) are often tempted to do.
The authors did, however, try to make excuses. Indeed, the shorter version of the whole discussion section seems to be: How can it possibly be that we didn’t find acupuncture to be superior to sham acupuncture for menopausal hot flashes?
They noted:
Our findings are consistent with those from a recent Cochrane review (10), which reported that acupuncture was more effective than no treatment and had a moderate effect size but was not efficacious when compared with sham. Although another recent meta-analysis reported moderate standardized effect sizes of acupuncture of −0.35 and −0.44 for HF frequency and severity (13), this analysis pooled data from sham-controlled trials and trials comparing acupuncture with no treatment. In addition, the shortcomings of the included studies (small sample sizes, high attrition rates, and failure to use intention-to-treat analyses) may have inflated the treatment effects.
I can’t help but note that “more effective than no treatment” + “not efficacious when compared with sham” = not efficacious.
This observation, of course, leaves the question of why bother to do this study in the first place, given that there’s enough evidence out there to do a Cochrane review and that review found no evidence that acupuncture was more efficacious in menopausal hot flashes than sham acupuncture, and that there was enough evidence to do a meta-analysis whose results were probably due to the inclusion of low quality evidence. There was (and is) no strong clinical or scientific rationale to do randomized studies of acupuncture for menopausal hot flashes.
This next paragraph made me chuckle out loud as I read it:
The first limitation of our trial and acupuncture clinical research more broadly is the lack of an inert sham comparison treatment. Although the Park sham device was the best available sham acupuncture method at the time of study design, its validity as an effective control treatment needs further determination. It creates a needle-prick sensation, essential for the patient to believe that a needle has been inserted; however, this sensation produces minor physiologic effects (26). The interpretation of sham-controlled acupuncture trials must occur within this context. However, what we have successfully examined is the effect of needling compared with pressure from a blunt needle. Second, despite our broad recruitment strategy, our findings can only be generalized to Caucasian Australian women with kidney yin deficiency. Nonetheless, 87% of otherwise eligible women met criteria for symptoms of kidney yin deficiency, consistent with previous studies (17, 18). Third, our method of Chinese medicine diagnosis was a simplified version of usual practice and failed to define secondary diagnoses. In addition, our acupuncturists could not be blinded, but we provided comprehensive training and performed quality assurance visits to minimize bias. Finally, our findings cannot be generalized to women with bilateral salpingo-oophorectomy or worsening of VMSs after breast cancer; we excluded these women because they have more severe VMSs (47, 48). Future research should examine the role of acupuncture in breast cancer.
Yes, let’s count the excuses, which sound increasingly desperate. One: The sham needles weren’t an adequate control. (Never mind that they’ve been used in many studies and found to be quite good.) Two: Our findings can’t be generalized to all women with menopause but only to Caucasian Australian women who also—by the way—have kidney yin deficiency. (Are they saying that menopause is so different in other races that this result can’t be generalized? That’s even leaving aside the insistence on an unvalidated, pre-scientific method of diagnosis.) Three: Our method of traditional Chinese medicine diagnosis was too simplified. (If only we could have brought all our woo diagnosis criteria to bear, there’d have been a positive result!) Four: Our acupuncturists couldn’t be blinded. (Actually, this one deficiency with the study was in the investigators’ favor and made a seemingly “positive” result more likely. They didn’t get one.) Five: We can’t generalize our findings to women with menopause due to surgery or to breast cancer treatment. So let’s study the role of acupuncture in alleviating menopausal symptoms in breast cancer patients! (Stay tuned for the next study I discuss here.)
So once again, we have yet another study that shows that acupuncture doesn’t work, and once again we have investigators who refuse to believe their own results and have to be dragged, kicking and screaming, by the data to the conclusion that their hypothesis was false. Even then, they can’t help making lots of excuses and planning their next study even though this one was totally negative.
Same as it ever was. So is the next study, which turns the normal rationale for using a good “sham” or placebo intervention in a clinical trial on its head.
Acupuncture and menopause: Acupuncture “works,” but only compared to nothing
There’s already sufficient evidence out there (e.g., studies like this one) to show that acupuncture doesn’t work for menopausal symptoms in breast cancer patients undergoing treatment with anti-estrogen drugs and/or chemotherapy (which can also induce menopausal symptoms); that is, other than studies that don’t bother to blind anybody. This has not prevented, for example, the Society for Integrative Oncology from including acupuncture in its clinical guidelines for breast cancer patients. Nor did it stop what is considered to be one of the top journals for oncology, The Journal of Clinical Oncology (or, as we affectionately call it, JCO), from publishing a study like this one conducted in Italy, “Acupuncture As an Integrative Approach for the Treatment of Hot Flashes in Women With Breast Cancer: A Prospective Multicenter Randomized Controlled Trial (AcCliMaT),” by Lesi et al from the Unit of Medical Oncology Civil Hospital. The study was published as an Epub Ahead of Print late last month and even featured a week ago in the ASCO Connection, which is the news outlet of the American Society of Clinical Oncology, one of the largest oncology professional societies in the world.
AcCliMaT is what we in the biz like to call a “pragmatic” trial. Those who have been regular readers of SBM know what “pragmatic” means in this context. Basically, pragmatic trials are clinical trials designed to test how well an intervention that has already been validated in rigorous randomized controlled trials (RCTs) works in “real world” situations. The key assumptions behind a pragmatic study design are that we already know that a treatment works and that we are examining how well it works outside the tightly controlled environment of a clinical trial. Why do pragmatic trials? Simple. It’s because often in the real world treatments don’t work as well as they do in RCTs due to many reasons, including, for example, application of the treatment to patients who wouldn’t have met the inclusion criteria of the RCT, less rigorous adherence to the treatment protocol, and patient noncompliance.
Of course, doing a pragmatic trial is putting the cart before the horse for treatments that have not been shown to work through rigorous RCTs, but that’s exactly what AcCliMaT does. In fact, the rationale for AcCliMaT almost made me spew the iced tea I was drinking as I wrote this all over my MacBook Pro’s screen. Check out the interview with one of the study’s co-authors, Giorgia Razzini, in ASCO Connection:
According to study coauthor Giorgia Razzini, PhD, the strength of the study published in JCO is its rigorous and pragmatic design. Previous studies have compared acupuncture for hot flashes to “sham” or non-optimal acupuncture, with the goal of controlling for the therapeutic response that might arise from patients receiving increased attention and a laying on of hands (i.e., the placebo effect). However, this study compared acupuncture to the treatment women with breast cancer would actually receive in clinic, that is, self-care. To further strengthen the study’s design, the acupuncturists paid great attention to minimizing behaviors that could potentially contribute to a placebo effect.
“The acupuncturists worked with a multidisciplinary team of oncologists and clinical trial managers to share their expertise and their knowledge and made an effort to standardize the acupuncture as much as possible to reduce the placebo factors present in many complementary medicines. In fact, acupuncturists delivered the intervention without talking to the patient, or at least keeping the talking to a minimum. The study was conducted with extreme attention to trying to minimize the placebo effect,” said Dr. Razzini.
There’s so much wrong here and only so much verbiage even I can devote to it. The key misconception at the root of this study is simple. Razzini seems to assume that placebo effects derive only from patient interaction, the “laying on of hands,” and the like. No doubt these are important contributors to placebo effects, but it’s nonsense to think that placebo effects can be minimized so much by not having the practitioners talk to the patients that a comparison of an intervention + self-care to self-care alone wouldn’t still yield a positive result. It will, and, not surprisingly at all, in this study it did. Basically, this study had no good control group and failed to control for placebo effects, given that everyone involved was unblinded and knew which group each subject was in. It’s also unclear what, exactly, was done to minimize interaction. All it says in the paper is this: “Conversation between acupuncturists and patients was kept to a minimum to limit nonspecific treatment effects.”
So basically, this study was a randomized controlled trial of two interventions. The first is “enhanced self-care”:
To standardize usual care recommendations, we enhanced self-care by providing all patients with a detailed information booklet about climacteric syndrome management. The booklet (Appendix, online only) was developed by the research team after a consensus process and included details about hot flashes and cancer and recommendations on diet, physical exercise, and eventual psychological support. The content of the booklet was explained to all patients before random assignment, and booklets were then distributed. Patients were asked to follow self-care recommendations for at least 12 weeks from random assignment.
So basically, the control group was given a booklet and told to follow its recommendations. I wonder how well that usually works out. (Hint: Not very.)
The experimental group received enhanced self-care plus acupuncture:
Within 2 weeks of random assignment, in addition to self-care recommendations, the acupuncture group was offered 10 traditional Chinese medicine (TCM) acupuncture sessions once per week for 12 weeks. The treatment protocol identifies six TCM menopausal syndromes according to Maciocia’s recommendations (Table 1).22 At the beginning of each acupuncture session, a TCM evaluation of the tongue and radial pulses was performed to identify the prevailing syndrome and consequently choose appropriate acupoints in addition to three common acupoints (ie, SP 6, LI 11, CV 4). Patients received 20-minute acupuncture treatments based on the diagnosed TCM syndrome; moxibustion was provided as per TCM diagnosis. In some cases, supplementary points were punctured, but no more than 11 acupoints were used for each session. Sterile disposable 0.30 × 0.40 mm Huan Qiu needles (Suzhou Huanqiu Acupuncture Medical Appliance, Suzhou, People’s Republic of China) were inserted bilaterally to a depth of 0.5 to 1 cm in most areas, except the hip, where the depth was 1 to 2 cm. They were manually manipulated to elicit the de qi sensation. No flicking or rotation of the needle took place once inserted. Participants with lymphoedema were not treated in the affected arm. No other complementary therapy was recommended during the course of acupuncture.
Here’s a hint. In any study of nothing (in essence) versus nothing plus an intervention, the nothing plus intervention group will almost always come out on top, because it’s not just the patient-practitioner interaction that is responsible for placebo effects. It’s the intervention itself, the more invasive, the more powerful the placebo effects. It’s not as though this isn’t known and hasn’t been studied, including how more costly sugar pills induce stronger placebo effects. It’s even known that sham surgery is the most powerful placebo of all. This study was, whether intentional or inadvertently, designed to produce a positive response to acupuncture. It could hardly do otherwise.
And that’s what happened.
A total of 190 women with breast cancer were randomly assigned. Inclusion criteria included, but were not limited to: diagnosis of breast cancer, age 18 to 65 years, intention to continue hormonal treatment at least through the length of the study, mean number of six or more hot flashes and/or daily mean score of 15 or greater on the Greene Climacteric Scale (GCS) during the week before enrollment, and vasomotor syndromes for at least 6 weeks. Some exclusion criteria included: treatment of climacteric syndromes such as systemic phytoestrogens, tibolone or analog, veralipride, or specific homoeopathic drugs and use of hormone replacement therapy and/or antidepressant drugs in the previous month and no intention to discontinue. The primary outcome measure was the hot flash score at week 12 (end of treatment), which was calculated as the frequency multiplied by the average severity of hot flashes. Secondary outcomes measured included climacteric symptoms and quality of life, measured by the Greene Climacteric and Menopause Quality of Life scales. Outcomes were measured for up to 6 months after treatment.
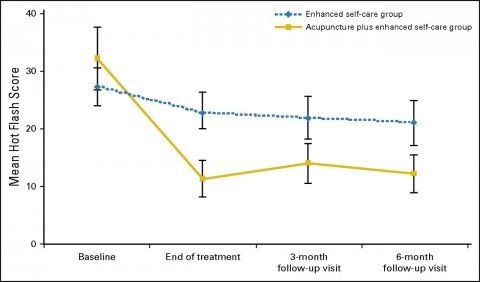
The results, which are utterly unsurprising given the trial design, are summarized in this graph:
The authors also found that women in the acupuncture plus enhanced self-care group reported a higher quality of life in terms of vasomotor, physical, and psychological symptoms, with most scores on the various measures being around 25%-30% improved compared to the control group.
Based on these utterly unsurprising results, the authors concluded:
In conclusion, AcCliMaT—a multicenter pragmatic trial with a standardized TCM acupuncture protocol—confirmed that acupuncture is an effective and safe intervention for severe menopausal symptoms in women with breast cancer. Further research could help to identify which variables predict treatment response and the optimal duration of acupuncture. Because these findings seem both statistically and clinically meaningful, we hope the practice of treating vasomotor symptoms in women with breast cancer will change.
No, what this trial found is that the acupuncture group did better than the control, but we have no way of knowing if this result was due to placebo effects or not because there was no sham acupuncture control. Of course, the authors know that their results don’t show that acupuncture works better than sham acupuncture. They even admit it:
We acknowledge that this design does not allow estimation of the size of the effect resulting from needling itself or from other placebo-related factors, such as patient−provider interaction. Attempts were made to balance and control the potential impact of the latter by providing both groups with a booklet about climacteric syndrome management options and ensuring that therapists in the acupuncture group limited the communication and time spent with patients to the minimum needed for quality treatment. Notably, study participants did not differ in acupuncture response expectancy.
“Attempts were made…” Sure, utterly inadequate attempts. I could have saved the authors a whole lot of money and effort and predicted the results just by reading the study protocol. Sadly, no one asked me. I will say right now, though: Anyone thinking of designing a similar study, drop me an email or call. I’ll predict the results. And JCO editors: The next time you get a manuscript describing a trial like this, consider me (or Steve Novella) as a reviewer. Your peer reviewers dropped the ball big time on this one, as did your publicity department for writing up a glowing article about this study.
The bait and switch continues
It’s not as though we didn’t already know that acupuncture doesn’t work for menopausal symptoms, either. For instance, a systematic review published in JCO in 2013 found no benefit for acupuncture for any cancer-related symptom other than chemotherapy-induced nausea and vomiting (CINV), all due to high risk of bias (ROB) in the studies included and evaluated. (Personally, I find the evidence that acupuncture helps with CINV unpersuasive, because it relied almost entirely on one trial with a low ROB and mixed electroacupuncture and acupuncture studies, but that’s a topic for another post.) Similarly, a Cochrane review from 2013 (noted above in the discussion of the first paper) also found no benefit over placebo. Yet none of this stops acupuncture advocates from believing that acupuncture works to alleviate menopausal hot flashes, be they natural or breast cancer treatment-induced, or from doing more studies like the two I just discussed.
We at SBM, particularly Steve Novella and I, have discussed on multiple occasions the ways that advocates try to make ineffective treatments seem effective and how they spin negative results as being positive, particularly how CAM advocates substitute low quality evidence for high quality evidence because high quality evidence shows that their interventions don’t work. In these two studies, we have a perfect representation of this. The Italian study, whose design was decent for a pragmatic study but assumed what lawyers would call facts not in evidence (i.e., that acupuncture works for hot flashes), produced a seemingly “positive result.” However, it did not adequately control for placebo effects. (An understatement!) When investigators do control for placebo effects adequately, as the Australian investigators did, the results show that acupuncture has no detectable specific effects greater than placebo. This is often much to the disappointment and consternation of the investigators, as the contortions the Australian group went through in its Discussion section illustrate rather amusingly.
Overall, there is no convincing evidence that acupuncture is anything but elaborate, theatrical placebo. The Australian study is quite consistent with this conclusion, and the Italian study provides no evidence to refute it. The Australian investigators, their attempts to explain their negative results notwithstanding, do deserve at least some praise for having followed the results of their study where they led. In contrast, the editors at JCO and ASCO itself should be ashamed for having published and promoted this study.